Deductibles, Out-of-Pocket Healthcare Spending Rose 3% in 2015
Payers need to invest in value-based care such as bundled payments and accountable care organizations in order to minimize the rise in healthcare spending.

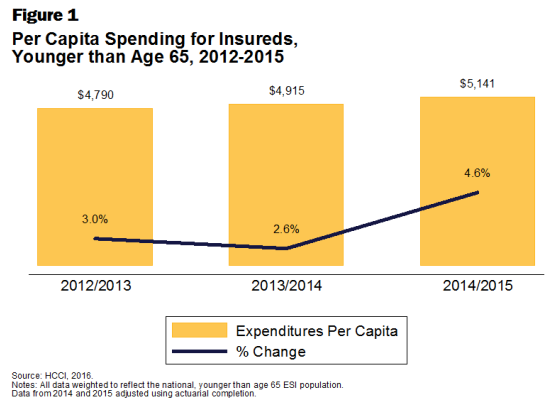
- Healthcare spending within the private health insurance market has grown 4.6 percent in 2015, according to a press release from the Health Care Cost Institute (HCCI). This type of growth in spending is higher than in recent years. For instance, healthcare spending in 2014 saw a 2.6 percent rise while 2013 spending increased by 3 percent.

The HCCI study, called the 2015 Health Care Cost and Utilization Report, shows that the costs for prescription drugs, outpatient services, and inpatient care rose anywhere from 3.5 to 9 percent last year. These cost increases are significantly larger than prior years, which led to both patients and health payers taking on more of the reimbursement cost.
The report found that the main reason for these cost growths were due to providers increasing their prices. The Health Care Cost Institute looked at medical claims data from 2012 to 2015 among four national payers, which include Humana, Aetna, Kaiser Permanente, and UnitedHealthcare.
“Spending grew faster than we might have expected in 2015, given the slower growth in previous years,” said HCCI Senior Researcher Amanda Frost. “The combination of people using more health care services and the faster growth in prices pushed up spending, with prices playing the bigger role.”
Healthcare spending for consumers under 65 years of age with employer-sponsored coverage rose to an average of $5,141 per person in 2015. In fact, out-of-pocket spending as well as the costs of deductibles and coinsurance grew 3 percent last year, averaging out to $813.
“Using data from four of the nation’s largest health insurers, we’re able to look closely at the changes in health care use and prices over time to understand what is driving costs,” explained HCCI Executive Director David Newman. “Year after year in our study period we see that rising prices are leading to spending growth.”
The results show that older patients above 40 years of age spent more than $1,000 out-of-pocket in 2015 while women spent an extra $236 out-of-pocket than men on average.
The study also separated healthcare spending between different states. The results show that the District of Columbia and Maryland had the lowest out-of-pocket spending while Texas had the highest at $983 on average.
There was a slight rise in the use of doctor visits, lab tests, and other professional services in 2015. However, other healthcare items like prescription drug use, emergency room visits, and surgical hospital admissions declined in use last year. The study also noted that visits to primary care practitioners decreased between 2012 and 2015 at an average annual rate of 4.7 percent.
The total healthcare spending for emergency room visits grew 10.5 percent in 2015 while the prices of professionally administered medication rose 12.5 percent to an average of $534. The costs of an acute hospital admission rose around $1,000 each year of the HCCI study. In 2015, the price of acute hospital admissions $19,967 on average.
While healthcare spending seems to be on the rise, there are a number of steps that payers can take to reduce these costs. For instance, implementing the bundled payment model could help incentivize providers to cut wasteful spending.
When it comes to hip or knee replacement surgeries, cancer screenings, and some other forms of treatment, bundled payment models enable payers and providers to gain cost savings. Health IT tools, digital technologies, and mobile health apps can also play a role in decreasing healthcare spending.
For instance, telehealth capabilities could enable more doctors and specialists to communicate quickly and streamline the process of diagnosing patients. Physicians can also use telehealth to provide quick and efficient care to their patient base.
In a previous interview, Pamela Coffey, Chief Clinical Officer at HealthSmart, provided input on how payers could reduce healthcare spending related to emergency room visits and hospitalizations.
“To really get a handle on [reducing healthcare costs], you have to identify why these services are being used,” noted Coffey. “Oftentimes, it’s because of a lack of primary care in that healthcare scenario. My recommendation is that you have the data that let’s you identify what are the features and factors in that healthcare scenario that make them high risk. Data is key.”
“You need to identify what the cause of the emergency room use is or the hospitalization, which tends to be an exacerbation of a situation that if it had good, sound primary care to begin with, they would seek out the care of their primary care physician or their specialist rather than going to the emergency room or having their condition degrade to where a hospitalization is necessary,” she concluded.
Additionally, investing in accountable care organizations over the long-term has shown to bring in cost savings and reduce overall healthcare spending. Payers can follow these key steps to ensure future years don’t see a spike in medical costs.
Dig Deeper:
How to Overcome the Challenges of Bundled Payment Models
What Are the Benefits of Accountable Care Organizations?