Does Blocking State Medicaid Expansion Create a Coverage Gap?
Halting state Medicaid expansion left some individuals above eligibility for this type of health insurance and below the limit for tax credits through the health insurance exchange.

- The most recent data on state Medicaid expansion shows that a total of 20 states are declining to broaden Medicaid coverage among those living below poverty level.

One of the provisions under the Patient Protection and Affordable Care Act meant to expand healthcare coverage to the uninsured has been the push toward state Medicaid expansion. However, several years ago, a Supreme Court ruling determined that state Medicaid expansion would be a voluntary action. This led to a number of states halting the spread of Medicaid coverage.
This means that Medicaid coverage within these states is offered to a family of three only if their annual income is no more than $8,840 while childless adults are left without even these provisions, according to a report from The Henry J. Kaiser Family Foundation.
The report explains one of the problems with halting state Medicaid expansion is that some individuals fall into a coverage gap in which their incomes are above eligibility for this type of health insurance and below the limit for tax credits through the health insurance exchange.
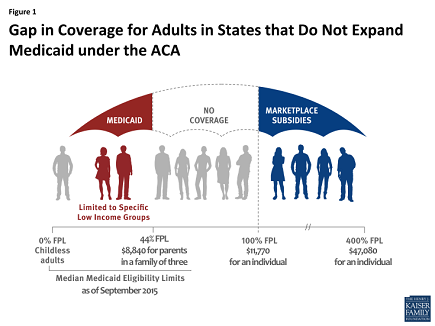 Currently, approximately three million uninsured adults fall into this particular coverage gap, the report explains. However, this gap could be completely closed if the states choose to broaden Medicaid coverage across their borders. Out of all people who fall into the coverage gap, 25 percent reside in Texas, 18 percent in Florida, 10 percent live in Georgia, and 8 percent are from North Carolina.
Currently, approximately three million uninsured adults fall into this particular coverage gap, the report explains. However, this gap could be completely closed if the states choose to broaden Medicaid coverage across their borders. Out of all people who fall into the coverage gap, 25 percent reside in Texas, 18 percent in Florida, 10 percent live in Georgia, and 8 percent are from North Carolina.
The results also showed that 90 percent of those falling into the coverage gap come from southern states. The lack of coverage limits this population from pursuing healthcare services when in need of medical attention. This may essentially block healthcare access among the uninsured.
The report goes on to explain that if state Medicaid expansion actually took place in the 20 states that decline to broaden this type of insurance, approximately 5 million Americans would become eligible for healthcare coverage.
“The ACA Medicaid expansion was designed to address the high uninsured rates among low-income adults, providing a coverage option for people who had limited access to employer coverage and limited income to purchase coverage on their own,” the report from the Kaiser Family Foundation stated.
“However, with many states opting not to implement the Medicaid expansion, millions of uninsured adults remain outside the reach of the ACA and continue to have limited, if any, option for affordable health coverage: they are ineligible for publicly-financed coverage in their state, most do not have access to employer-based coverage through a job, and all have limited income available to purchase coverage on their own.”
“State decisions about Medicaid expansion have implications for the potential scope of Medicaid under the ACA. If all states expanded their Medicaid programs, eligibility for Medicaid in non-expansion states would grow from just over half a million to 5.5 million,” the brief continued.
“Medicaid is designed to provide a safety net of coverage for low-income people, with benefits and provider networks targeted to this population and coverage available throughout the year as people’s circumstances change. There is no deadline for states to opt to expand Medicaid under the ACA, and debate continues in some states about whether to expand. If more states adopt the expansion, the coverage gap will shrink and more low-income adults will gain access to Medicaid eligibility.”
While it is important to discuss the coverage gap among the uninsured, it is also vital to cover the reasons behind why certain states decided not to expand their Medicaid programs. A report from the Center on Budget and Policy Priorities mentions that a number of governors refuse to expand Medicaid because it would place a “financial burden on their states.”
However, these claims may not be completely valid, the report states. The Congressional Budget Office determined that the amount of money spent on expanding Medicaid coverage would be offset by no longer needing to cover uncompensated care offered to the uninsured such as through free clinics.
The analysis shows that the federal government will also be handling nearly 93 percent of the costs associated with state Medicaid expansion and the individual states will increase healthcare coverage spending by 2.8 percent. However, these states will also experience cost savings in other areas of healthcare due to the provisions of the Affordable Care Act, the report from the Center on Budget and Policy Priorities proposes.
There are some who claim more individuals who are already eligible for Medicaid under current law will enroll in the coverage option if additional states will expand their Medicaid programs. These opponents feel that state budgets will suffer from the expansion.
Nonetheless, the report from the Center on Budget and Policy Priorities details how state Medicaid expansion would offer healthcare coverage among 17 million low-income consumers at a low cost to the individual states, which will also be offset by eliminating the need for uncompensated care and state-funded programs for uninsured citizens.
Additionally, it is important to mention that the federal share of state Medicaid expansion is $931 billion or 93 percent of total costs while states will need to cover $73 billion or 7 percent of the remaining costs.
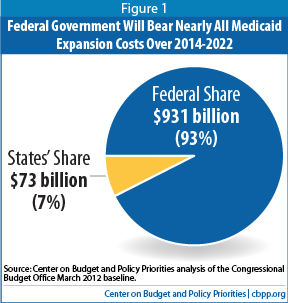
“Contrary to claims made by some of the Medicaid expansion’s critics, the expansion does not impose substantial financial burdens on states. The additional state Medicaid spending that CBO expects to result from the expansion equals 2.8 percent of what states would have spent on Medicaid in the absence of health reform; this estimate includes the cost of covering individuals who are currently eligible but not enrolled,” the report concluded.
“CBO expects that the expansion will result in 17 million more people being covered, which will significantly reduce state costs for uncompensated care and related programs and offset some or potentially all of the increase in state Medicaid costs.”
