Healthcare Bundled Payments, Silver Plan Changes Impact Payers
As the federal government invests more resources in reforming reimbursement, healthcare bundled payments are expected to become a more mainstream part of provider revenue.

- The federal government especially the Department of Health and Human Services (HHS) and the Centers for Medicare & Medicaid Services (CMS) have targeted healthcare payment reform in an effort to reduce rising medical costs around the nation. In January 2015, the HHS Secretary Sylvia M. Burwell announced that 30 percent of fee-for-service Medicare payments will need to be in the form of alternative payment models such as healthcare bundled payments or shared savings through accountable care organizations by the end of 2016.

“Today’s announcement will be remembered as a pivotal and transformative moment in making our health care system more patient- and family-centered,” Debra L. Ness, president of the National Partnership for Women & Families, stated in an HHS press release.
“This kind of payment reform will drive fundamental changes in how care is delivered, making the health care system more responsive to those it serves and improving care coordination and communication among patients, families and providers. It will give patients and families the information, tools and supports they need to make better decisions, use their health care dollars wisely, and improve health outcomes.”
In addition to the goals for 2016, Burwell expects at least half of Medicare payments to be in an alternative payment arrangement by the end of 2018. Using the Hospital Value Based Purchasing and the Hospital Readmissions Reduction Programs, HHS plans to link up 85 percent of fee-for-service Medicare payments to quality care standards by 2016 and 90 percent by 2018.
“Employers are increasingly taking steps to support the transition from payment based on volume to models of delivery and payment that promote value,” Janet Marchibroda, Health Innovation Director and Executive Director of the CEO Council on Health and Innovation at the Bipartisan Policy Center, said in a public statement. “There is considerable bipartisan support for moving away from fee for service toward alternative payment models that reward value, improve outcomes, and reduce costs. This transition requires action not only by the private sector, but also the public sector, which is why today’s announcement is significant.”
As the federal government invests more resources in reforming medical reimbursement, healthcare bundled payments are expected to become a more mainstream part of provider revenue. At the end of 2015, HHS announced in a press release the Comprehensive Care for Joint Replacement (CJR) model, which will be a platform for healthcare bundled payments set to begin on April 1, 2016.
With hundreds of thousands of Medicare beneficiaries obtaining knee and hip replacements on an annual basis, CMS and HHS are working to lower the costs associated with these surgeries by adopting healthcare bundled payments.
“Today, we are embarking on one of the most important steps we will take to improve the quality and value of care for hundreds of thousands of Americans who have hip and knee replacements through Medicare every year,” HHS Secretary Sylvia M. Burwell stated in the release. “By focusing on episodes of care, rather than a piecemeal system, we provide hospitals and physicians an incentive to work together to deliver the best care possible to patients.”
Complication rates after these surgeries at some hospitals are higher than at others while the costs can vary by half when considering hospitalization, the operation itself, and recovery time. Hospitals in 67 geographic areas will be required to follow the bundled payment model set up by the Comprehensive Care for Joint Replacement program in order to improve quality and medical spending outcomes.
Those who have strong outcomes will be provided with extra reimbursement while those who fall below performance benchmarks may have to repay Medicare for some of the spending related to these surgeries.
As the federal government continues to focus on reforming healthcare payment, the likelihood for improved quality of care and cost savings is expected to advance. Health Affairs reported on one instance in which bundled payments led to savings in healthcare spending.
Blue Cross and Blue Shield of North Carolina (BCBSNC) adopted a bundled payment model for knee replacements, which consisted of a seven-month period. The pilot program showed that Blue Cross and Blue Shield saved anywhere from 8 to 10 percent for single-episode costs.
While payers and providers focus on implementing bundled payments to stabilize their healthcare spending, the federal government is searching for ways consumer costs can be decreased. New proposed regulations for health insurance plans in 2017 seeks to lower out-of-pocket costs for consumers while improving access to certain medical services and prescription drugs.
Essentially, all cost-sharing will have to be the same across identical level plans offered by multiple insurers. The government is also calling for payers to sell at least one silver package plan.
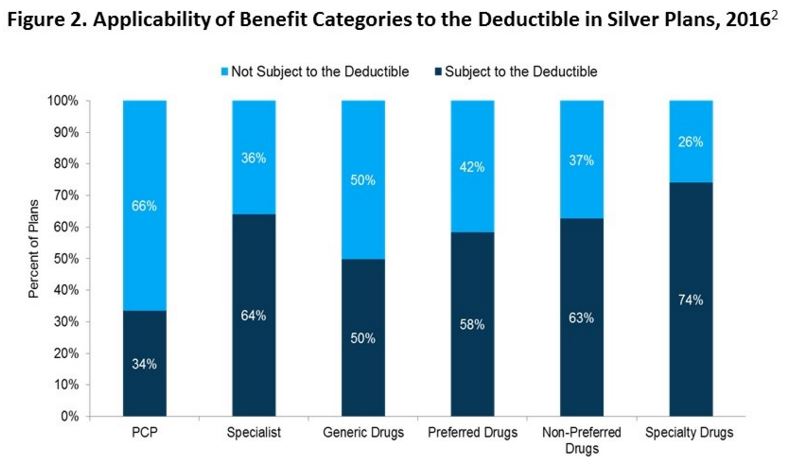
The new structure would offer physician visit coverage requiring immediate co-payments and insure all tiers of prescription drug costs among silver and gold plans. Currently, silver-level plans on the health insurance exchange have very high deductibles averaging out to $2,889 in 2016.
This could lead many consumers to pay well over $2,000 on top of their premiums when seeking medical care. Specialty visits and specialty drugs are often part of this deductible. These proposed regulations, however, could change all this.
“Introducing standardized benefit designs into the federal exchange builds on the existing approach of many states,” Elizabeth Carpenter, vice president at Avalere, said in a public statement. “While standard benefits limit flexibility for plans and could increase costs, the structure may appeal to some consumers by making it easier to compare plans and choose insurance.”
As the federal government positions new regulations and prepares the Medicare program for healthcare bundled payments, the entire industry from payers to providers is expected to reach the Triple Aim of better patient satisfaction, improved health outcomes, and more stabilized spending.
Image Credits: Avalere Health