How Care Management Strategies Could Reduce Medical Costs
Due to a growth in the number of chronic medical conditions around the United States, health payers are working to develop care management strategies that will better serve patients with complex diseases.

- When it comes to managing the treatment and financial implications of complex medical conditions, health payers and providers will need to work together and have effective cross-industry communication. A strong relationship between payers and providers is a must in order to create superior care management strategies for at-risk patient populations.

Due to a growth in the number of chronic medical conditions around the United States, health payers are working to develop care management strategies that will better serve patients with complex diseases, according to a white paper from the California HealthCare Foundation.
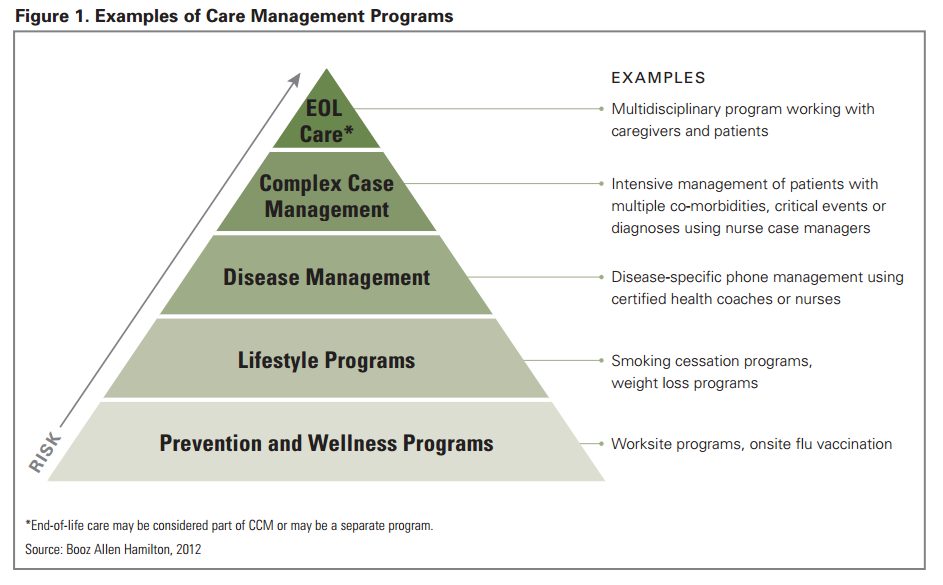
Payers are developing Complex Case Management programs for helping patients with acute and critical health problems and Disease Management programs for those who have more common chronic conditions.
In order to fit the requirements of new legislative actions such as the Affordable Care Act, payers and providers are working to re-design some of these programs, the white paper stated.
Health payers are now more focused on population health management including disease prevention and wellness promotion. For example, beneficiary incentives are meant to spark consumer interest in obtaining all health screenings, managing medication dosages, and remaining physically fit.
The white paper discusses how patients in the state of California have experienced a spike in chronic diseases such as diabetes. With approximately 40 percent of Californians suffering from one or more chronic conditions, payers are more interested than ever before in developing effective care management strategies with their network of providers.
Private, commercial payers have several methods for developing care management strategies including Complex Case Management and Disease Management. For example, one method may be contracting with an outside vendor to develop a care management approach while another way would be to develop the strategy in-house.
There are several approaches in care management programs such as consumer outreach and engagement along with provider engagement and risk stratification. A survey conducted by the California HealthCare Foundation shows that two-thirds of California payers use in-house services for developing Complex Case Management and Disease Management strategies.
Cammack Health reverses cost trends through care management
One example of a health payer and provider network that worked to reverse rising healthcare spending through the development of effective care management strategies comes from consulting company Cammack Health and Montefiore’s health plan, according to a company press release.
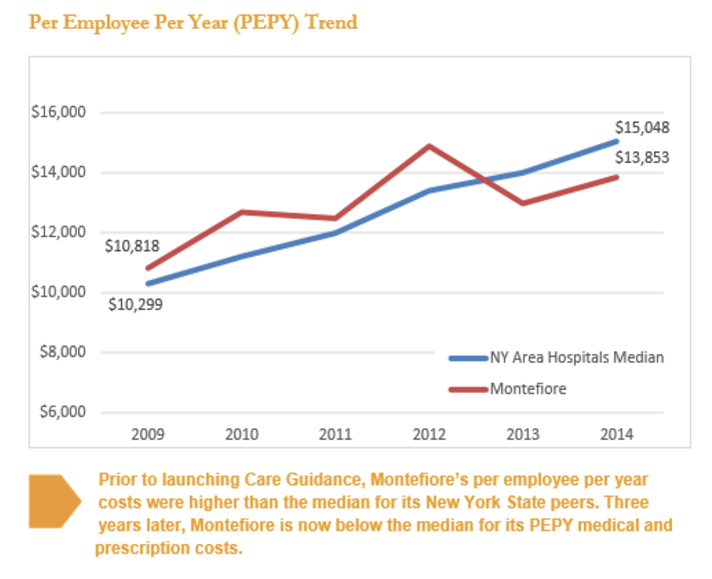
In 2011, it was discovered through Cammack Health’s annual Benefits Survey of Hospitals that the costs associated with the Montefiore health plan were above average per employee per year when compared to New York hospitals.
In order to solve this major dilemma, Cammack Health, Montefiore Health System’s Human Resources department, and Montefiore’s nationally recognized Care Management Organization (CMO) partnered together to create a Care Guidance Program along with redesigning plan benefits and coverage options.
Four years ago, Montefiore’s per employee per year health plan spending was $12,475 while the average for New York hospitals was $11,982. The three parties used the care management platform at the CMO to create the Care Guidance Program.
“We understood some people might view this kind of program cynically, as simply a means of managing claims. But it’s not being done by the claims administrator; it’s being done by a separate entity,” William Shanahan, former Vice President of Human Resources at Montefiore, said in a public statement.
“This, plus the fact that the program is voluntary, sends a clear message to employees that the program is here to help you and your dependents, not to mandate you to do anything. From what we’ve heard anecdotally, this approach has worked to reassure people.”
The way this program works is by targeting health plan members to follow a healthy lifestyle and better navigate the medical care system when issues arise. Also, the Care Guidance Program is meant to find at-risk patients early before a health concern exacerbates and provide wellness education for them. All of these steps are meant to stabilize the costs of healthcare at this particular establishment.
This program also lasers in on care coordination and disease management in order to stabilize medical spending within the Montefiore health plan. Those with chronic conditions are offered services through a Personal Health Nurse.
The nurse works with individuals in order to promote medication adherence and other healthy behaviors. One important point to mention is that the majority of plan members favor the program and are interested in its goals.
“The concern was that people would see the program as Big Brother or invading their privacy,” Anne Meara, RN, Associate Vice President of Network Care Management, mentioned in the press release. “Yet the majority of people we contact are very appreciative of an offer for help. The program has generated significant goodwill, positive word of mouth and even referrals from coworkers participating in the program.”
The results show that the new program has led to significant benefits such as the drop in spending by around $1,000, a report from Cammack Health shows. Engaged consumers and plan members saw their medical as well as prescription drug costs fall by 10.8 percent since 2011.
Some other benefits included a decrease of utilization in “key categories, including a 19.6% reduction in inpatient admissions, 26.7% reduction in non-maternity-related inpatient admissions, and 13.4% reduction in emergency department visits.”
This illustrates that strong care management strategies between provider networks and payers could lead to a stabilization in medical costs across multiple organizations.
“We were looking for some mechanism to help us moderate the trend in healthcare costs, rather than simply shifting costs from employer to employee,” William Shanahan explained in the report.