How New Policies Impact Healthcare Spending and Access
There were some important findings uncovered in these studies including that healthcare spending around cancer treatment rose because outpatient practices became consolidated.

- The Health Care Cost Institute (HCCI) announced today the publication of six different policy briefs entailing how state and federal regulations are affecting healthcare spending and patient services. Independent researchers used HCCI’s claims data on more than 50 million insured consumers around the nation, according to a press release from the organization.

There were some important findings uncovered in these studies including that healthcare spending around cancer treatment rose because outpatient practices became consolidated. This may be due to additional fees that outpatient facilities charged insurers. Consolidation also led to the use of more innovative and pricey medications.
“We are pleased to be a data resource for independent researchers who can drill down into the issues that impact our nation’s health,” HCCI Executive Director David Newman stated in the press release. “This research builds on the national reporting and analysis that HCCI continues to focus on in its own work.”
Physical therapy cuts healthcare spending
The policy briefs also included information about the benefits of “unrestricted access to physical therapy.” Regular physical therapy sessions seem to reduce the reliance on opioids and lowers healthcare spending overall.
Specifically, when it comes to lower back pain, visiting a physical therapist as the first form of treatment may reduce future costly services such as emergency room visits and prescription opioid use. The researchers looked at patients who sought physical therapy first and found that their pharmacy care, physician, hospital, and outpatient services were lower when compared to patients who spoke with a different healthcare provider first.
Primary care costs drop with nurse practitioner use
In another policy brief, it was uncovered that greater utilization of nurse practitioners leads to reduced costs associated with primary care. The researchers looked at independent scope-of-practice laws, which allow nurse practitioners to treat their patients without a physician present in the room. Costs of primary care were found to decrease by 1 to 4 percent.
“Currently, we have limited information on the effects of reforms happening at the state and national levels,” HCCI Senior Researcher Amanda Frost said in a public statement. “We believe that this data-driven research will build a knowledge base about the changing healthcare landscape, and serve as a resource for policymakers and consumers alike.”
Telehealth reimbursement declines
Researchers from the University of Nebraska Medical Center’s College of Public Health discovered that telehealth reimbursement from private payers was about 40 percent lower than reimbursement for in-person medical care. The number of claims related to telehealth services doubled from 2009 to 2013 among primary care offices, but the medical claims continued to be paid at lower amounts when compared to in-person services.
The problem at hand may be that only seven states have passed parity laws that require telehealth services to be reimbursed at identical levels to non-telehealth visits. As such, while private payers are required to reimburse these technology-based virtual visits, insurers are not mandated to pay at the same levels as other similar forms of medical care.
“The gap between telehealth and non-telehealth reimbursements of primary care providers are likely to discourage major investments in telehealth technologies by clinics unless these technologies result in substantial cost savings to clinic operations,” the policy brief stated. “As of July 2015, only seven states (Arkansas, Delaware, Hawaii, Minnesota, Mississippi, Tennessee, Virginia) have mandated that private insurer reimbursements for telehealth services be comparable to those for covered non-telehealth services.”
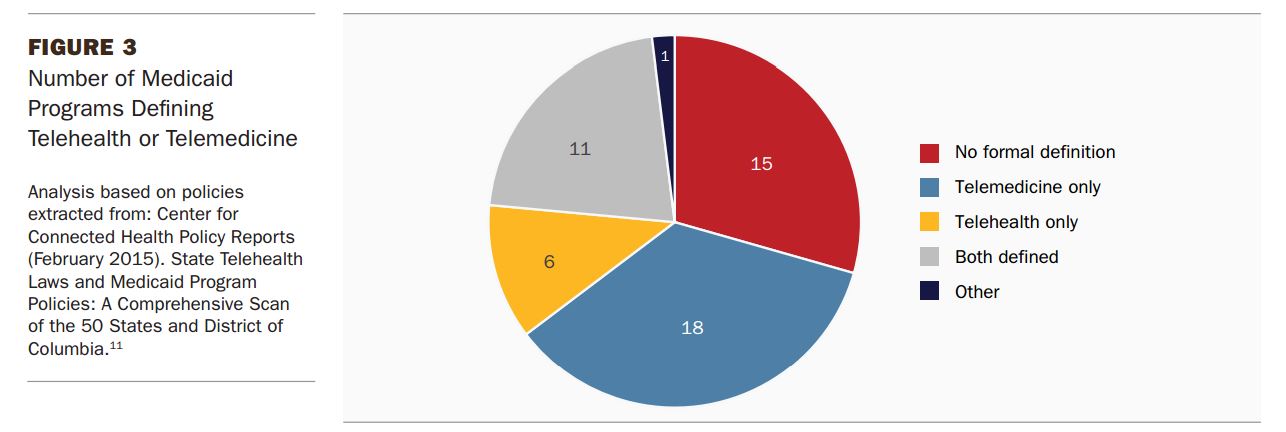
Despite the fact that state Medicaid programs have adopted telemedicine reimbursement, the definition of telehealth and telemedicine seems to vary greatly and lack uniformity among Medicaid coverage plans.
Even though more and more providers are offering and using telehealth services, it seems that medical claims to private payers involving telemedicine is rather rare. Additionally, low reimbursement rates for virtual care could lead to decreased adoption of telemedicine and new technologies, the policy brief stated.
Mental health parity laws have little effect on healthcare access
Experts from the University of Colorado School of Medicine published a policy brief outlining how the Mental Health Parity and Addiction Equity Act has done little to truly expand access to mental healthcare services.
The researchers looked at patients with depression, schizophrenia, and bipolar disorder and found that the Mental Health Parity law “had little to no effect on access and use of mental health services.” In particular, the study looks at the utilization of mental health services before the parity laws were introduced in some states and compares it to the use of psychiatry or psychology after parity was established.
Before the parity laws became established in this country, health plans often had limited visits and restrictions on type of mental healthcare services available, which led to fragmented care, less satisfaction, and worse health outcomes.
Due to this, a handful of states passed laws requiring more coverage equality between physical medical care and mental health services. The Affordable Care Act also brought more parity between these types of services by including parity in the health plans sold through the federal exchanges.
The amount of visits to mental health providers, however, did not increase after the Mental Health Parity and Addiction Equity Act took effect, the study discovered. Essentially, the policy brief indicates that mental health parity laws did not have the effect hoped for.
As the nation continues reforming the healthcare field and payment systems, state and federal regulators may need to better address some of the current issues related to reimbursement and healthcare spending.
Image Credits: Health Care Cost Institute