How Risk-based Bundled Payment Arrangements Boost Quality
Healthcare providers are being required by Medicare to transition to more alternative payment models such as pay-for-performance initiatives and bundled payment arrangements.

- Bundled payment arrangements are slowly being recognized by providers and payers as methods for reaching the Triple Aim – quality care improvements, lower costs, and better health outcomes. Some consulting companies are even educating their clients on contracting through bundled payment arrangements. For example, the healthcare consulting company ECG Management Consultants has established a bundled payments practice to the services it offers, according to a company press release.

“Since beginning this work in 2010 and seeing evidence that our methods truly do reduce healthcare costs and improve clinical outcomes, we’ve had a growth mind-set,” Deirdre Baggot, Ph.D., M.B.A., R.N., a national bundled payments expert, said in a public statement. “My team members and I are disruptive innovators at heart, so ECG’s entrepreneurial spirit was an obvious fit as we looked to expand our capabilities. Having spent the last six years studying, building, and testing bundled payment constructs, we are bursting with enthusiasm for the opportunity to scale our work in a meaningful way.”
Now that healthcare providers are being required by Medicare to transition to more alternative payment models such as pay-for-performance initiatives and bundled payment arrangements, this new service offered by ECG Management Consultants should be useful among clinicians.
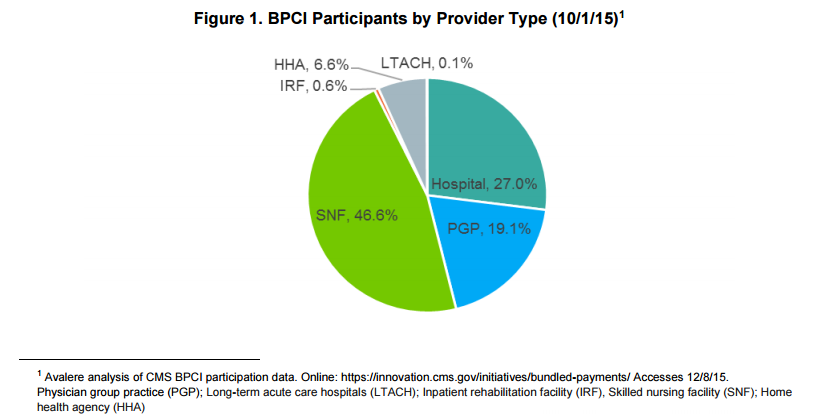
This is especially important in a time when providers are unsure about whether to pursue risk-based bundled payment arrangements. For instance, an analysis from advisory firm Avalere Health shows that participation in the Centers for Medicare & Medicaid Services’ (CMS) voluntary Bundled Payment for Care Improvement (BPCI) has dropped from the initial interest expressed among healthcare providers.
The current number of participants is only 25 percent of the original amount of providers interested in the Bundled Payment for Care Improvement program. Nonetheless, 1,500 participants are partaking in the program as of October 1, 2015.
The drop in participation is troublesome and will show whether CMS continues to provide voluntary programs or will create more mandatory bundled payment arrangements similar to the Comprehensive Care for Joint Replacement (CJR) program.
“Strong participation in a voluntary program shows providers’ willingness to test new alternative payment models,” Josh Seidman, Senior Vice President at Avalere. “However, the fact that many providers that entered the program decided it’s not currently in their financial interest to accept downside risk may cause CMS to consider additional mandatory programs in the future.”
Within the Bundled Payment for Care Improvement program, providers have to assume clinical and financial risk when contracting with CMS. Skilled nursing facilities are the most common providers taking part in the program and are followed by hospitals and physician group practices.
In today’s economic climate, providers should pursue risk-based contracting with payers in order to ensure healthcare costs decrease and quality improvement across the medical spectrum is achieved.
For instance, value-based care reimbursement and pay-for-performance initiatives aim to reduce hospital readmission rates, medical errors, and hospital-acquired infections while boosting the number of cancer screenings conducted and greater care coordination between facilities.
The Healthcare Financial Management Association (HFMA) released a report outlining risk-based financial models among payers and providers, according to a company press release. A number of healthcare payment models are discussed including Pioneer Accountable Care Organizations, pay for performance reimbursement, and episodes of care bundled payments.
To begin with, it’s important to understand that the healthcare industry is shifting toward value and away from fee-for-service reimbursement. The federal government is pushing for higher quality care and greater patient satisfaction while commercial payers are focused on developing risk-based payment systems.
The consumers, on the other hand, have been facing higher premiums and deductibles, which is bringing a greater demand for price transparency and systems in place to lower the costs of care.
More consumers are seeking cost-effective solutions for their medical services, which is why providers and payers should seek out risk-based bundled payment arrangements expected to keep healthcare spending low.
At this moment in time, providers are slowly contracting with payers through alternative payment models. Risk-based contracts essentially offer providers a system of either gaining or losing reimbursement based on health outcomes and quality measures.
“Providers, payers, and other organizations are increasingly entering into contracts or assuming new payment models that expose the parties to the uncertainty of financial gain or loss,” HFMA President and CEO Joseph J. Fifer, FHFMA, CPA, said in a public statement. “All organizations that are involved in risk-bearing arrangements must ensure that their accounting practices keep pace with their contractual obligations as they evolve.”
Bundled payment arrangements offer providers reimbursement for a specific episode of care, which could include treatment among a multitude of physicians and medical facilities. Over time, alternative reimbursement solutions such as bundled payments will likely bring better quality of care, improved health outcomes, and decreased spending across the healthcare spectrum.
Image Credits: Avalere Health