Physician Compare Website Upgrades Benefit Medicare Population
Currently, the Hospital Compare online tool includes more than 100 quality measures across 4,000 hospitals around the country.

- Medicare and Medicaid beneficiaries along with consumers of plans via state health insurance exchanges gained an advantage last week when the Centers for Medicare & Medicaid Services (CMS) announced website improvements to the Physician Compare and Hospital Compare tools.

Medical facilities, Accountable Care Organizations, and individual physician practices will need to address some of the new quality measures introduced by CMS to the Physician Compare website feature. The measures address the quality of care among providers serving Medicare beneficiaries along with other patients.
The Hospital Compare website feature was also updated with several new measures and extra information. Currently, the Hospital Compare online tool includes more than 100 quality measures across 4,000 hospitals around the country.
“Consumers want trustworthy, reliable, and understandable information about the quality of health care delivered by providers,” CMS Deputy Administrator and Chief Medical Officer Patrick Conway, M.D., MSc, said in a public statement.
“Both Physician Compare and Hospital Compare show consumers that they have a choice. This large release of quality measures for hospitals and physicians empowers consumers with information to make more informed health care decisions, encourages health care professionals to strive for higher levels of quality, and drives overall health system improvement.”
Medicare and Medicaid beneficiaries can take a look at the Physician Compare feature and examine the quality measures surrounding preventive care, diabetes and cardiovascular treatment, and patient safety standards among the providers participating in the Physician Quality Reporting System. Currently, CMS posted quality measure data for about 275 group medical practices taking part in the Physician Quality Reporting System.
The quality measures will help Medicare recipients decide which provider would offer them the best possible services in their region based on their particular healthcare needs. Additionally, there is now data on patient experience scores among some medical practices available on the Physician Compare website tool.
Via the Consumer Assessment of Healthcare Providers and Systems (CAHPS), CMS was able to post information on patient experience performance scores among about 290 group medical practices for beneficiaries to view. These practices asked their Medicare recipient base to provide feedback on their healthcare experience.
Additionally, this is the first time that consumers would be able to look at performance scores of individual physicians and professionals with regard to preventive and cardiovascular care as well as patient safety standards.
CMS has also provided information on Accountable Care Organizations, specifically 2014 clinical care quality and patient experience performance measures among 20 Pioneer ACOs and 333 ACOs participating in the Medicare Shared Savings Program.
Essentially, the Hospital Compare and Physician Compare features are meant for helping consumers make the best decisions about the medical care they need from Medicare providers and other healthcare facilities. Over the years, the number of facilities and doctors reporting data on quality performance measures has risen steadily due to new legislative actions and reforms.
One new measure for inpatient quality reporting included determining whether a hospital uses safe surgery practices during an entire operating procedure including anesthesia provisions, during incisions and closing, and before a patient leaves the operating room. Some more information on hospital-acquired infections was also made available via these CMS website tools.
Reporting these quality measures to allow consumers to compare their options is vital for both the payer and provider markets. The Physician Quality Reporting System is vital in “driving healthcare quality improvement,” according to a CMS report.
CMS will be working toward enhancing its quality reporting programs in order to overcome the current challenges of quality improvement in the healthcare market. Currently, CMS is seeking greater feedback from stakeholders including patients, caregivers, and medical professionals as it continues to work on strengthening its quality reporting systems.
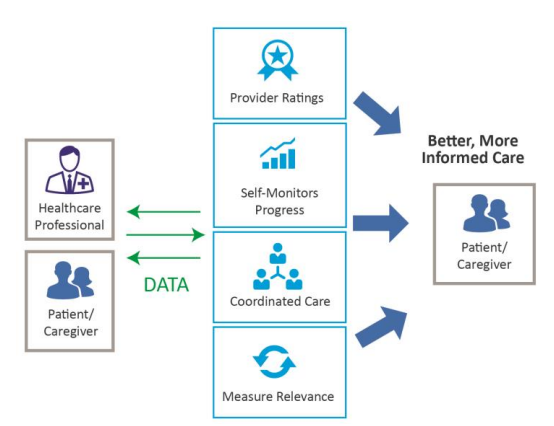
This type of feedback can stimulate a general cycle of quality improvement. Additionally, it’s vital for stakeholders to have a system or infrastructure in place for leveraging performance data and implementing strategies to improve their quality scores. The graphic below illustrates a general feedback and data-driven cycle that leads to quality improvement.
Value-based reimbursement models must also align with quality performance standards in order to offer real benefit to healthcare quality improvement measures. With the help of health IT tools and health information exchange, more rapid changes will take place in enhancing the quality of care among medical practices and hospitals as well.
“We are living in a time of unprecedented change for health IT. Initiatives like the Medicare and Medicaid Electronic Health Records (EHR) Incentive Programs are at the forefront of hospitals, physicians and nurse practitioners to adopt an electronic medium for patient information,” Kate Goodrich, Director Center for Clinical Standards & Quality, wrote for The CMS blog.
“CMS and physicians have a shared goal in the EHR program of helping physicians, clinicians, and hospitals to deliver better care, smarter spending, and healthier people.”
Technology can help providers monitor quality performance measurements continually at the direct point of care. CMS is looking to work on strengthening health IT within its own programs as well as through other federal agencies and the private sector.
“CMS envisions a future where technology provides seamless support to quality improvement efforts. Technology can enable quality improvement in a variety of ways, such as by providing feedback on performance against quality 6 measures in real time,” the report stated.
“CMS recognizes that outcomes measures rely on multiply sources of data and may not support the timely access of data in the near future; however, CMS will continue to look for ways to align performance measures with clinical decision support tools, so that these point of care tools directly support the quality improvement driven by its quality measures.”
Image Credit: Centers for Medicare & Medicaid Services