Premier Accountable Care Organizations Improved Quality in 2015
Accountable care organizations operating within the Premier Population Health Management Collaborative reduced spending and enhanced quality in 2015.

- New results from the Premier Inc. Population Health Management Collaborative (PHMC) show that accountable care organizations (ACOs) within the collaborative improved quality and cost reduction in 2015 better than other ACOs operating through Medicare, according to a company press release.

The study compared the results from the Medicare Shared Savings Program (MSSP) to that of the Premier Population Health Management Collaborative. Approximately 30 percent of MSSP accountable care organizations and Pioneer ACOs have qualified for shared savings while half of Population Health Management accountable care organizations have been deemed eligible for shared savings for a second year.
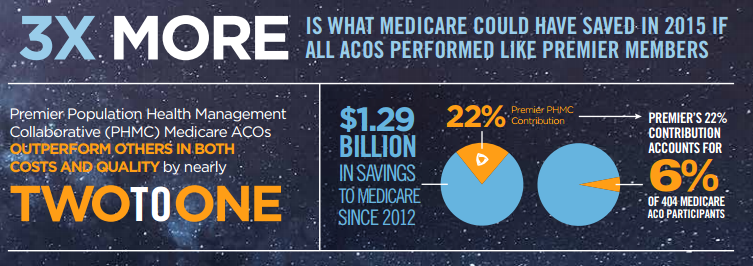
The Centers for Medicare & Medicaid Services (CMS) may benefit from bringing some of the achievements and capabilities of accountable care organizations operating within the Population Health Management Collaborative into other Medicare ACOs. In fact, Premier conducted an analysis that shows as much as $1.36 billion could have been saved in 2015 if every Medicare ACO reached the same cost and quality benchmarks as the Population Health Management Collaborative ACOs.
Had this cost savings actually taken place, the savings would be three times that of the $466 million shared across all 404 Medicare accountable care organizations. Even though the Population Health Management Collaborative ACOs take up only 6 percent of all Medicare accountable care organizations, these entities have brought in 22 percent of the cost savings since 2012.
“Succeeding within these models is challenging, but these results show that a shared mission, effective collaborative execution model, peer-to-peer benchmarking and performance improvement along the way can help some make the transition faster, with higher-quality outcomes,” said Melissa Gerdes, MD, Vice President and Chief Medical Officer of Outpatient Services and ACO strategy, Methodist Health System in Dallas. “Being an MSSP ACO participant in Premier’s collaborative has positioned Methodist as a leader in value-based payment.”
Premier also states that 80 percent of their accountable care organizations achieved shared savings in 2015 compared to 42 percent of ACOs that were also originally formed in 2012.
Private payers would benefit from learning about the success of Premier accountable care organizations. Learning what sets these particular ACOs apart from the rest could help payers and providers achieve similar cost savings and quality improvement efforts in future years.
When it comes to national quality scores, ACOs operating in the Population Health Management Collaborative reached 93.8 percent when compared to an average of 91.5 percent across the country.
The quality scores reached last year among PHMC accountable care organizations rose 6.5 percent since 2014. Members of the Population Health Management Collaborative and its ACOs reported five specific factors in which they succeeded garnering cost savings through alternative payment models.
The five factors include: better disease management, physician engagement, use of population health IT tools, well-structured post-acute care networks, and stronger in-network utilization management.
“PHMC members have demonstrated that smart planning, active physician leadership and professionally-managed implementation drives sustained quality and population health improvement,” said Joe Damore, vice president of population health at Premier. “These results are critical, particularly now that many providers are evaluating advanced alternative payment models under the Medicare Access and CHIP Reauthorization Act (MACRA). Even with benchmarks that are lower than the national average, these health system-sponsored ACOs are making an impact in a wide variety of communities across America and bending the healthcare cost curve.”
While private payers and CMS consider the factors that enable success in PHMC accountable care organizations, the federal government has also stepped forward with legislation meant to bolster Medicare ACOs.
In September, representatives Diane Black (R-TN) and Peter Welch (D-VT) proposed legislation that would transform some of the regulations around Medicare accountable care organizations. The proposed law, called the ACO Improvement Act of 2016, includes reforms for the Medicare Shared Savings Program such as waivers for telehealth site-of-service, cost-sharing for primary care treatment, and patient attribution.
With legislation and further commitment to reform the healthcare industry, stakeholders, payers, providers, and government agencies will likely lead accountable care organizations into a future of more cost reduction and quality improvements.
Image Credits: Premier
Dig Deeper:
What Are the Benefits of Accountable Care Organizations?
Time, Commitment Required for ACO, Value-Based Care Success