Primary Care Payment Reform Targeted in Multi-Payer Initiative
This is the first time CMS has targeted primary care payment reform on such a large scale.

- The Centers for Medicare & Medicaid Services (CMS) are renovating how primary care is delivered throughout the United States. According to a news release from the agency, CMS is launching a program called the Comprehensive Primary Care Plus (CPC+) model, which will be the federal agency's largest multi-payer initiative ever formed. This is the first time CMS has targeted primary care payment reform on such a large scale.

Approximately 5,000 primary care practices throughout 20 regions will be affected by this program. This means that 25 million patients treated by more than 20,000 physicians will be eligible to receive higher quality medical care while the physician practices undergo primary care payment reform.
The Comprehensive Primary Care Plus program will last for five years and is meant to help patients with serious medical conditions or chronic disease meet their health goals, explains the news release.
“Strengthening primary care is critical to an effective health care system,” Dr. Patrick Conway, CMS deputy Administrator and Chief Medical Officer, said in a public statement. “By supporting primary care doctors and clinicians to spend time with patients, serve patients’ needs outside of the office visit, and better coordinate care with specialists we can continue to build a health care system that results in healthier people and smarter spending of our healthcare dollars. The Comprehensive Primary Care Plus model represents the future of health care that we’re striving towards.”
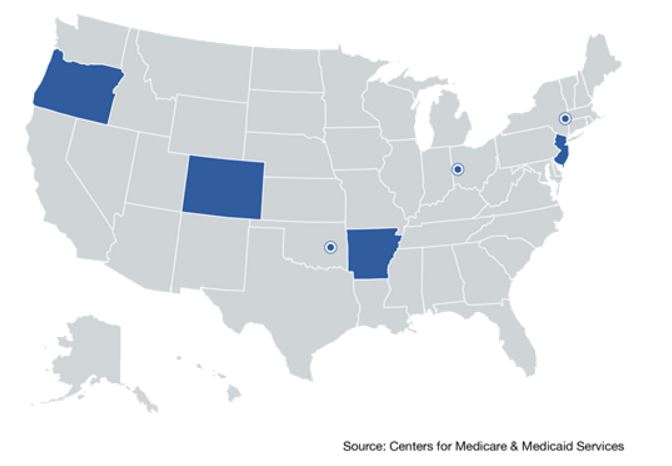
Reimbursement for this primary care payment reform model will be based on the results doctors achieve, the health outcomes of patients, and general quality care improvements. Initially, CMS created the Comprehensive Primary Care initiative in 2012. This program was meant to last four years and strengthen primary care payment reform through a multi-payer approach. The states that participated in the Comprehensive Primary Care initiative can be seen in the map below.
Primary care practices will also need to ensure that patients have access to 24-hours-per-day healthcare services as well as medical information. One important piece of the puzzle will be to provide preventive medical services such as screenings and blood work.
Both patient engagement and care coordination will be key for the success of primary care payment reform within this CMS model. Primary care physician offices will participate in two different tracks. Both tracks will cover the above criteria, but Track 2 “will also provide more comprehensive services for patients with complex medical and behavioral health needs,” according to the release. These patients will receive psychological assessments and be connected to resources that will help meet their behavioral health needs.
Primary care practices working through Track 1 will be given a monthly fee by Medicare for their managed care activities as well as standard fee-for-service reimbursement. For those in Track 2, however, primary care practices will receive up-front comprehensive primary care funds and a reduced fee-for-service reimbursement amount along with a monthly managed care payment.
The news release explains that this hybrid model of payment will allow providers to offer Medical Care that varies from the standard face-to-face doctor's visit, which could include telemedicine utilization, remote medical monitoring, or home visits.
“CPC and CPC+ are both payment and care delivery models,” stated a report from The Journal of the American Medical Association (JAMA). “Similar to CPC, practices selected to participate in CPC+ will use defined, stepwise requirements to guide them through care delivery changes required to provide 5 comprehensive primary care functions: (1) access and continuity, (2) risk-stratified care management, (3) planned care for chronic conditions and preventive care, (4) patient and caregiver engagement, and (5) comprehensiveness and coordination of care.”
“Even though the original CPC model ends later this year, CMS will continue its rigorous evaluation of the final years of data to determine whether this model meets criteria for expansion. As one of the few primary care models with an incentive for practices to control cost, CPC will contribute significantly to current understanding of effective primary care model design.”
This CMS program is another initiative in which the federal agency strives to implement value-based care reimbursement and move away from the fee-for-service system. Department of Health and Human Services Secretary Sylvia M. Burwell has established a goal of bringing 50 percent of Medicare payments toward alternative reimbursement models by the end of 2018.
Medicare and partnering health payers will offer financial incentives for primary care providers to participate in this revolutionizing program. As the practices continue to boost their patient care outcomes, they will either be allowed to keep these financial incentives or be penalized monetarily if they haven’t met quality performance measures.
The new primary care payment reform model will bring commercial health payers to work together with Medicare in order to strengthen the delivery of services within this particular healthcare field. The most important aspect of the Comprehensive Primary Care Plus program is that it further transitions medical practices toward adopting new payment models focused on pay-for-performance protocols and mutes the focus on fee-for-service reimbursement.
As the federal government and the health insurance industry bring greater focus toward value-based care, medical providers will need to transition their revenue cycle management to handle these new payment models.