Top Challenges of Alternative Payment Models, Bundled Payments
Bundled payments can financially penalize doctors for essential services that were out of their control.

- The Center for American Progress released a report last Spring that tracks the progress and success of alternative payment models within the Medicare program. The report outlines that a one-size-fits-all strategy is not the right one to take when reforming Medicare reimbursement, according to a press release from the Center for American Progress.

The findings show that supporting the growth of bundled payment models over the short term could further help flourish accountable care organizations or ACOs. With Medicare, one of the nation’s largest health insurance program, operating on a fee-for-service platform, it further leads to an excess of waste and unnecessary spending on needless tests or even prescription drugs across the healthcare industry.
However, there is more momentum taking place at the Centers for Medicare & Medicaid Services (CMS) to move away from fee-for-service payment. In fact, CMS plans to tie at least half of reimbursement claims to alternative payment models within the next two years. ACOs along with bundled payment strategies are being adopted across the nation to lower costs and increase the quality of care.
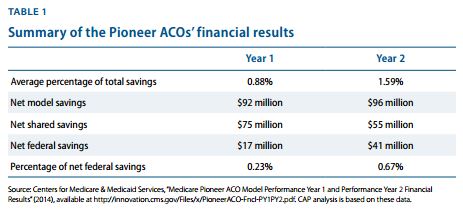
The report is called A Strategy for Medicare Payment Reform and seeks to better understand the progress of Pioneer accountable care organizations. Quality scores were calculated and federal savings were compared against performance quality benchmarks. The Pioneer ACO model showed slightly favorable results but hasn’t met the initial projected goals of the Medicare Shared Savings Program.
For example, federal savings only met 0.67 percent of the initial ACO benchmark goals. Additionally, most savings tend to be gathered in a clump among a few accountable care organizations instead of spread throughout these models of care. However, data shows that Pioneer ACOs improved their quality performance during the second year of practice when compared to the first year the model of care was implemented.
Why bundled payments offer more promise than ACOs
“A careful look at the data CMS released for Year 1 and Year 2 of the Pioneer ACO program paints a modest but improving picture,” the report stated. “The data show that, overall, Pioneer ACOs provided quality care and improved their quality scores from Year 1 to Year 2. As CMS reported, the average score for 28 out of 33 quality measures increased from Year 1 to Year 2, while the average improvement across all quality measures was 14.8 percent. Twenty ACOs improved their score from Year 1 to Year 2 on at least 20 quality measures.”
“A review of specific programs shows that by changing incentives for providers to follow clinical-based practice guidelines, streamline vendor negotiations, and reduce unnecessary costs, episode-based bundles can increase value and improve care,” the report continued.
“While ACOs have attracted significant attention among Medicare payment reformers, bundled payment initiatives offer a chance for more immediate savings and quality improvements. As such, CMS should dramatically expand the use of bundled payments in Medicare.”
The report outlines methods for improving the effectiveness of accountable care organizations as well as implementing alternative payment models like bundled payments. The report encourages CMS to continue expanding the Bundled Payments for Care Improvement initiative around the country while also targeting the Medicare Acute Care Episode demonstration.
Alternative payment models like bundled payments and other value-based care reimbursement are much easier to implement throughout the nation due to the simpler administration and less cost requirements than that of accountable care organizations.
Obstacles of bundled payment strategies
The American Journal of Managed Care reported on the country’s move toward value-based care and alternative payment models such as bundled payments. While these new alternative payment models are meant to stimulate the healthcare industry in positive ways from improving the quality of care to eliminating wasteful spending, there are certain negative aspects to these new reimbursement strategies, Joshua T. Cohen, PhD, research associate professor of medicine at Tufts Medical Center mentioned to the news source.
In particular, bundled payments can financially penalize doctors for essential services that were out of their control. There are specific differences in patients affecting overall cost that the provider has no way to prevent or control.
For instance, some cancer patients could experience serious but rare complications from a chemotherapy drug that the provider would not have foreseen and would need to treat and address the side effects. The costs for these particular tests and treatments could not be based upon a bundled payment system.
Dr. Cohen also commented that certain factors like whether a patient adheres to a new diet, exercise regime, lifestyle change, or even prescribed medication is dependent upon the patients’ adherence and cannot be fully controlled by the physician. The providers will need to work with health payers to address the problems of reimbursing for services that are out of the control of the healthcare delivery system.
“There are situations where using a bundle may be inappropriate because the factors that are influencing differences in cost among patients are things that the provider doesn’t actually control. For example, you might have a range of patients who have different comorbidities, and some of them are very high risk, and hence would be expensive and that’s not the fault of the provider. And sometimes they are things that can be controlled by the provider. And sometimes, you can’t even tell. That’s what really makes things complicated,” Dr. Cohen explained.
“Looking further down the road, say we’re going to reimburse providers and we want to create a bundle for weight control. Well there it’s really obvious that there are matters outside of the control of the provider since the greatest predictor of whether a lifestyle change or a diet is going to work is the adherence by the patient. It’s not the different type of diet that’s prescribed. So the success there is definitely out of the control of the provider—it’s probably not a good candidate for a bundled payment.”
While the bundled payment system and alternative payment models aimed at value-based care are an important part of reforming the medical field, there are certain disadvantages that will need solutions in the coming years in order to create more robust bundled payments.