Why Health IT is Critical for an Accountable Care Organization
It is important to address whether some accountable care arrangements have the right type of health IT infrastructure to support the health data sharing aspects of coordinating care among multiple medical facilities.

- In order to provide medical services under an Accountable Care Organization (ACO), a network of medical practices, specialty healthcare offices, and hospitals must contract with a health payer such as Medicare, Medicaid, commercial health plans, or an employer-based insurance plan. The way an Accountable Care Organization functions is by having several groups coordinate care for a defined patient population and analyze certain health outcomes as well as quality performance measures, according to the Office of the National Coordinator for Health IT.

If an Accountable Care Organization spends more cash flow than the level set by the health payer, they will be at risk of losing these funds. Also, in order to participate in earned savings, the ACO will need to meet certain care quality metrics. If it fails to meet the metrics, the ACO will have to forfeit their savings.
However, if an Accountable Care Organization meets quality metrics and provides care at a lower cost than set up by the health payer, they are able to share in the savings with the payer. Some examples of successful accountable care programs come from the Medicare Shared Savings program, multi-payer ACOs, and Medicaid.
In order to meet some of the performance expectations, it could also be useful for providers within an ACO to support greater interoperability between multiple hospitals, clinics, and medical practices. When attempting to join an ACO, a healthcare provider could show their commitment to quality care at lower cost by implementing interoperable health IT products or participating in a health information exchange platform.
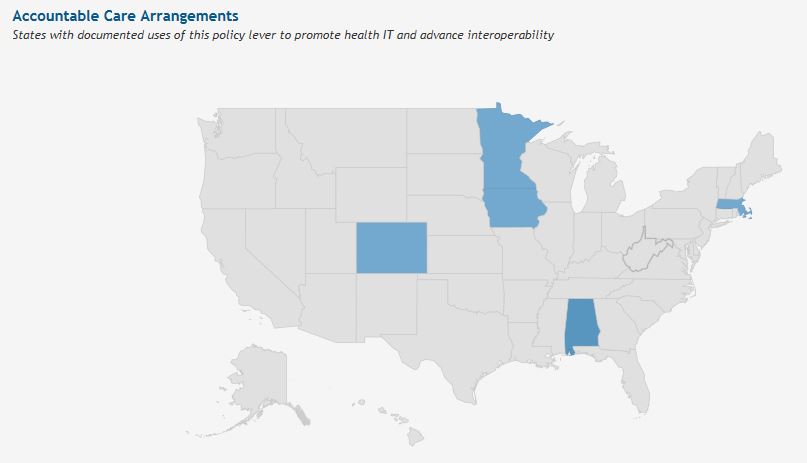
Some providers could gain more rewards or greater savings after demonstrating the implementation of interoperable health IT systems and participating in an Accountable Care Organization. Currently, there is a small number of states that have taken on developing ACO models. The map below illustrates this fact.
The Office of the National Coordinator for Health IT released a report one year ago that detailed how health information technology could be used to better support an accountable care program. The report begins by explaining how the healthcare industry has been transformed in recent years with regard to how payment is conducted. Physicians and patients are being incentivized in remarkable ways to support more quality care at lower cost.
This includes moving away from fee-for-service payment models and embracing value-based care, which is where Accountable Care Organizations come in. Value-based contracts like bundled payments and the like create a completely new relationship between payers and providers.
It is important to address whether some of these accountable care arrangements have the right type of health IT infrastructure to support the health data sharing aspects of coordinating care among multiple medical facilities. Interoperability of health IT is a vital aspect for the accountable care arrangement. This includes participating in effective health information exchange protocols.
“Health information exchange allows patients, doctors, nurses, pharmacists, other health care providers, to appropriately access and securely share a patient’s vital medical information electronically—improving the speed, quality, safety and cost of patient care. Robust HIE is critical to conducting effective care coordination within an ACO’s immediate network, as well as being able to receive information on care that patients receive from providers outside of the network,” according to the Office of the National Coordinator for Health IT.
The report details how vital it is for an ACO to have information technology capable of following the continuum of care for each patient and study collected data through a population health management perspective. However, many ACOs have still not completely created an effective information management system among multiple providers and medical facilities. Care management protocols are also subpar, according to the ONC report.
“As providers and payers have gained experience with accountable care models over the past several years, observers have continued to recognize the critical need for appropriate IT solutions to support success,” the report stated. “A 2013 evaluation of early results from the Pioneer ACO program16 suggested that successful accountable care organizations should have the capacity to identify and follow beneficiaries across the continuum of care, and to analyze beneficiary data from a population perspective.”
The Certification Commission for Healthcare Information Technology (CCHIT) outlined specific steps that ACOs should take to improve their health IT infrastructure and better serve their patient population. These steps include ensuring all providers are able to access patient information across the continuum of care, assessing patient status and using risk stratification to determine which patients need more intensive care, and leverage health IT tools to better engage patients and caregivers with their medical treatment.
The electronic medical record has become an imperative tool in the accountable care arrangement, as it collects pertinent patient data and medical history that doctors need to access in imperative situations. It is a vital piece of technology in the pursuit of patient safety.
“The healthcare industry has historically invested less in technology than other industries, but government regulations incentivizing technology upgrades have spurred the next wave in information mobility for healthcare,” Lynne Dunbrak, Research Vice President of Connected Health IT Strategies at IDC Health Insights, said in a public statement. “The need to access the right data at a moment's notice is even more critical in the healthcare industry when patient care is at stake. As hospitals realize the benefits to population health, meaningful use gains and accountable care, they are steadily making investments to improve their workflows and IT infrastructure for greater access to information.”
While there are health IT tools that do support some workflows within an Accountable Care Organization, it is imperative to continue to incorporate new technologies to improve interoperability and care coordination across the country’s ACO programs.