Why State Medicaid Expansion May be Worthwhile for All
Along with monetary matches, there are multiple studies that find significant benefits from greater use of the Medicaid program.

- When the Supreme Court ruled that Medicaid expansion under the Patient Protection and Affordable Care Act is voluntary among the states, this set a precedence that allowed individual states to play partisan politics and withhold from financing the expansion of their Medicaid program.

Currently, only 28 states alongside with the District of Columbia have implemented Medicaid expansion across their regions. While on the outside it may be understandable to decline extending Medicaid services due to the associated costs, it is vital to remember that the federal government would cover 100 percent of the costs from 2014 to 2016 and drop off funding at 90 percent by the year 2020, according to The Brookings Institution.
Why reasons for declining expansion fall flat
Additionally, a report from the Center on Budget and Policy Priorities states that expanding Medicaid would not pose a “financial burden” on the states. Essentially, the extra funds necessary for Medicaid expansion would come from the prior financial assistance covering uncompensated care of the uninsured at free clinics.
“While many critics point to the large cost of Medicaid programs, one recent analysis indicates that Medicaid eligibility for children produces enough additional tax collections over the long term to approximately pay for itself. The study found that childhood Medicaid raised cumulative taxes paid, reduced government earned income tax credit transfers, and increased cumulative wages among females,” the Brookings Institution reported.
“The evidence therefore indicates that the benefits of Medicaid coverage are large and that the long-term public cost may at least be partly mitigated by higher tax recipients from beneficiaries over time, while non-expansion states are forgoing significant federal transfers. Given that an increasingly large share of government aid has been focused on the working poor instead of those with the lowest incomes, Medicaid expansion represents an opportunity to improve the welfare of those worst off as this group continues to recover from the Great Recession.”
Revenue changes to state Medicaid programs
The Brookings Institution states that six states that have expanded their Medicaid program also made some significant changes to this healthcare payment model. These changes include billing for insurance premiums, copayments, and monthly fees that fall to the wayside when consumers take part in a healthy lifestyle including smoking cessation and weight loss.
Indiana is one state that expanded their Medicaid program with some of these transformations to the payment model including “locking residents out of coverage for six months if they fail to pay premiums.”
The coverage gap
Among the 22 states that have not widened their Medicaid coverage, a significant gap exists when it comes to health insurance among a certain sect of low-income individuals. There exists certain families and citizens with income too high to qualify for their state Medicaid programs and income too low to qualify for premium subsidies on the federal health insurance exchange.
Many of these states only offer Medicaid coverage if a family of three has an annual income of $8,840 or less while adults without any children do not qualify for the Medicaid program at all. As many as 6.7 million uninsured adults fall into this coverage gap in 2016, the Urban Institute concluded.
“Some state officials worry that Congress may not sustain the high FMAP ACA provides for expansion, on which the above favorable fiscal analyses rely. These officials believe the federal government must someday focus on deficit reduction and, when it does, they fear it will have little choice but to cut ACA’s unusually high FMAP for low-income adults. Such fears can seem reasonable until one delves into Medicaid’s current budget situation and past budget history. The federal Medicaid budget contains many other places to cut,” the Urban Institute report read.
“Historically, Congress has cut almost any other part of Medicaid before lowering the federal share of Medicaid costs, largely due to bipartisan gubernatorial resistance.”
Increase in Medicaid enrollment
Before the Affordable Care Act propelled Medicaid expansion, there were various issues found in the Medicaid program. One example is that Medicaid enrollment was only at 62 percent among those eligible. However, the individual mandate requiring citizens to purchase health coverage or else risk a tax penalty has pushed forward much larger enrollment numbers in state Medicaid programs.
The Brookings Institution reports that Medicaid enrollment rose by 18 percent in 2014 with 69 million low-income Americans covered under the program by the end of the year. States that expanded their Medicaid programs saw enrollment increase by 25 percent while those states that refused to broaden coverage saw a rise of only 7 percent. One state that took part in Medicaid expansion – Kentucky – actually saw a 70 percent jump in enrollment numbers.
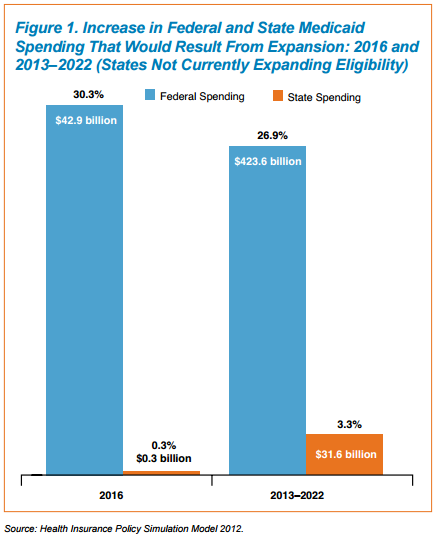
States that have declined to expand are also not accepting “$37 billion in federal matching funds and $14 billion in hospital reimbursement in 2016.” Besides the monetary matches, there are multiple studies that find significant benefits from greater use of the Medicaid program.
Clear benefits of state Medicaid expansion
For example, a report on Oregon’s Medicaid program shows that out-of-pocket expenses and debt are reduced while self-reported health outcomes are much better when compared to an uninsured population.
The Radiological Society of North America found another major benefit – Medicaid expansion led more low-income women to obtain recommended breast cancer screenings when compared to the populations of states that haven’t broadened their Medicaid coverage.
The researchers used the 2008 and 2012 Behavioral Risk Factor Surveillance System to view data on breast cancer screenings and establish that, before the Affordable Care Act’s provisions took hold, the rates of screenings were the same among the differing states. Then the investigators looked at data after the Medicaid expansion took place, finding that low-income women in states that expanded this type of coverage were 25 percent more likely to receive mammography.
“Adoption of Medicaid expansion by more states can result in considerable improvement of disparities in breast cancer screening, leading to better health outcomes for all women across the United States,” the study's lead author, Soudabeh Fazeli Dehkordy, M.D., M.P.H., from St. John Providence Hospital, said in a public statement.