How Payer Forecasting Is Shifting Towards Real-Time Data Analytics
A real-time data analytics approach demands that payers pursue full interoperability and requires a different mindset than the traditional approach has required.

Source: Getty Images
- As aggregators of healthcare data, payers are modern-day seers for the healthcare industry and they are increasingly leaning on real-time analytics to perform this role.
“Forecasting is a capability and an enabler to help create resilience in the broader businesses of payers,” Gurpreet Singh, US health services leader at PricewaterhouseCoopers (PwC), explained to HealthPayerIntelligence.

Gurpreet Singh, US health services leader at PricewaterhouseCoopers
Source: PricewaterhouseCoopersIn 2020, however, traditional methods of forecasting often fell short. Historical data could do little to guide organizations through the throes of the coronavirus pandemic. Macro-level fluctuations in elective care utilization and care venues created a healthcare year like no other in modern history.
Forecasting lay at the heart of both the drive towards resilience and the gravitation towards digitization, Singh said. Without an accurate view of the horizon, healthcare organizations would be unable to steer through the pandemic.
As a result, technologies that drew on real-time data became even more key to payers’ predictive efforts.
“Now the majority of health systems and payers have invested more significantly in predictive types of modeling and using automation techniques—both on the robotic process side of automation as well as the intelligent automation side—to drive some better insights,” shared Singh.
It is clear that predictive analytics is a top priority for healthcare leaders. According to PwC’s “Top Industry Issues of 2021” report, 74 percent of health executives said that their organizations would be investing in predictive modeling in 2021.
But in order for these technologies to keep up with current events, these predictive models may have to evolve to incorporate real-time data.
According to Singh as well as Josh Goode, chief information officer at SCAN Health Plan, and Gui Woolston, vice president of clinical analytics, analytics, and behavior change at CVS Health, the shift to real-time data analytics will require payers to adopt a new mindset about data analytics and a renewed fervor for interoperability.
Common uses for real-time forecasting
Payers are using real-time data to make predictions in various areas of the healthcare industry.
For example, real-time data analytics can help payers forecast shifts in membership.
When the economy fluctuates, payers may see increased churn between employer-sponsored health plans, the Affordable Care Act marketplaces, Medicaid, and Medicare. This migration between health plans can impact several payer functions, the least of which is their medical loss ratios.
Enrollment churn was a chief factor in payers’ mixed attitudes toward 2021 premium filings. Some payers increased premiums based on their predictions that changes in insurance status would lead to higher healthcare costs, a Kaiser Family Foundation report discovered.
Thus, having real-time data to project the amount of churn and assess the implications proved key for payers.
“The other aspect where real-time data can be effective is to try to understand how demand is changing so that you can better create the right capabilities around it,” Singh shared.
If payers can pinpoint when a particular service is in higher demand, they can innovate more precisely to address that consumer need. This data can also support payers as they determine how to reimburse for certain services such as telehealth.
“After having more of this real-time data, payers are going to be better equipped to understand whether virtual care and remote patient monitoring are truly lowering the cost of care and, therefore, reimburse appropriately,” Singh noted.

Josh Goode, chief information officer at SCAN Health Plan
Source: SCAN Health PlanGoode and his team at SCAN Health Plan have found real-time data to be most useful and accessible when it comes out of their own core-admin system—which collects enrollment, billing, and claims data—and the payer’s own contact centers.
For example, during the coronavirus pandemic, the health plan used language processing to isolate trends in member calls to the payer’s call center. The technology identified that members were frequently inquiring about coronavirus vaccinations. As a result, the payer could quickly adjust its messaging to help guide members to vaccine-related information on its website.
Another use for real-time data analytics is to monitor prescription choices. Aetna uses this strategy to ensure that members do not fill out a prescription that is inappropriate for their condition or that conflicts with other prescription drugs that the individual may be using simultaneously, Woolston said.
CVS Health has been working toward using real-time data to improve pharmacy transactions and member practices even before the company acquired Aetna, based on the belief that real-time data can help prevent adverse drug events, improve medication adherence, and cut costs.
Technologies for real-time predictive data
Two kinds of technologies are needed for using real-time data in predictive strategies. There are technologies that are necessary for collecting the data and tools that analyze the data.
Technologies that gather data will be real-time sensors. These may be physically closest to the member, Goode noted, particularly when used in remote patient monitoring.
For example, a blood glucose monitor that is in contact with a member can send member data via Bluetooth to an app. The app then gathers that data.
One of the major challenges though is the step between data collection and data analysis because it requires that payers have an open door to sensitive patient data.
“There are many technologies that are necessary to create integration,” said Singh. “Interoperability is a big topic as of late because a lot of data tends to be locked in EHRs. Or might be locked into a diagnostic device. Being able to integrate and pull data in a real-time fashion out of those locked boxes is one domain of technology.”
Once the payer has access to this data, it is time to analyze it so that the payer can draw conclusions and take action. At this stage, payers will often choose to lean into machine learning. They will also need to develop algorithms and storage capabilities for the unstructured data.
This approach allows computers to take over the “what is happening” question, leaving humans to answer the “why is it happening” question, Singh explained.
Challenges of real-time predictive data
Real-time data analytics requires a philosophical shift.
“It's a new way of thinking,” Goode explained. “There is a little bit of change management as you work with your business users around how you approach doing machine learning artificial intelligence, versus building traditional analytics.”
As opposed to traditional analytics models in which users have to manually tell the model what to do, users of machine learning artificial intelligence models have to define an overarching goal and then teach the model how to achieve the goal.
As a result, leveraging machine learning artificial intelligence models for predictive analytics and real-time analytics can change the way that a payer perceives its own goals and metrics for success related to forecasting.
Woolston added that there has been an evolution of the initial question at the core of data analytics processes which payers must ask themselves.
“We are increasingly moving beyond just predicting things (e.g. ‘will this member have a hospitalization next month?’) to predicting impactability, given our set of interventions (e.g. ‘will a member have a hospitalization that we could have helped him or her avoid next month?’),” Woolston said.

Gui Woolston, vice president of clinical analytics, analytics, and behavior change at CVS Health
Source: AetnaIn terms of procedural challenges, the data acquisition process is a key step that can hinder health plans from gathering real-time predictive data.
SCAN Health Plan uses application programming interfaces (APIs) with its partners to collect data in a near real-time way. Instead of getting batch files from SCAN Health Plan partners such as lab and pharmacy vendors at the end of the day, partners can use the payer’s APIs to push data to SCAN Health Plan almost as soon as the data becomes available.
“In order to drive real-time analytics, you first need to develop a real-time analytics data acquisition strategy and architecture that will ensure you have the most up to date data,” Goode explained.
Cost can be another obstacle for payers. Real-time data models require more maintenance than traditional models, Goode noted.
“This can be a costly endeavor for an organization as it may require investment in new technologies like an API management platform, in particular for acquiring external data sources, as well as looking at replication technologies that allow you to replicate data real-time from your online transaction processing (OLTP) systems into your analytics platform,” Goode said.
“Data streaming technologies may also be required for internet of things (IoT) devices, which in healthcare are an integral part of any remote monitoring strategy, so your data acquisition strategy needs to be a cornerstone of your overall real-time analytics strategy.”
While the costs may seem inhibitive, payers and healthcare executives across the industry have already been preparing to invest more in predictive analytics in general.
More than nine in ten payers viewed predictive analytics as important for the future of the industry in 2019, according to a survey conducted by the Society of Actuaries. At the time, six in ten healthcare executives, including payers’ executives, expected to put 15 percent or more of their budget towards predictive analytics.
Although real-time analytics may require a greater investment, it is clear that payers recognize the crucial role these technologies play in achieving their goals.
The final challenge in real-time analytics that payers must recognize is that all predictive analytics models have their limits, Woolston said.
“We do not have a crystal ball,” he stated. “No algorithm is going to be perfect at identifying the future. We seek to continuously improve our algorithms by collecting better data including data that the member voluntarily provides to us, using better statistical techniques, and validating our algorithms on a larger population.”
Changes in partner relationships when using real-time data
Real-time data gathering is not a solo effort. It requires partnerships between multiple stakeholders in order to piece together an accurate depiction of each member’s community. Payers have to collaborate with technology companies, providers, and pharmaceutical manufacturers to supply that information.
“Understanding the cost profile and what a community needs, almost down to the zip code level, is really necessary,” said Singh.
This is not new information to most healthcare executives. According to PwC’s “Top Industry Issues of 2021” report, 73 percent of healthcare executives said that they were collaborating or planned to collaborate with other providers and payers due to the pandemic. And 63 percent said that they were partnering with or planned to partner with public health entities.
Singh and the PwC report recommended establishing regional radars. These radars consolidate data from health information exchanges, hospitals, life sciences companies, and payers. These systems would not just pull from healthcare stakeholders, but also from sources with local economic data, demographic statistics, and behavioral information.
For this deployment of real-time predictive data through regional radars to become a reality, interoperability again comes into play. Just as it was necessary to have an interoperable structure in order for payers to access patient data, it is necessary to have an interoperable pathway for sharing data between stakeholders.
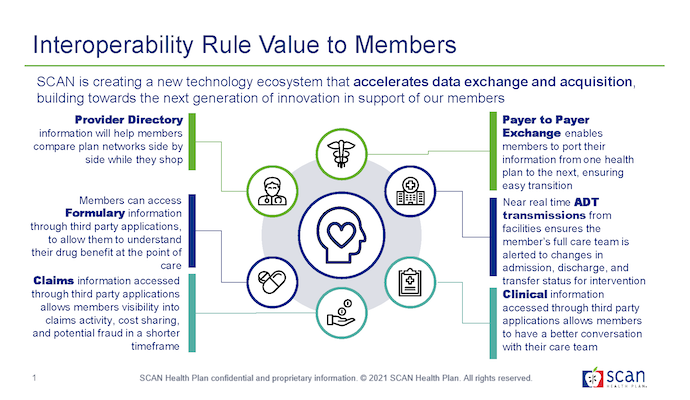
Source: SCAN Health Plan
That is why Goode was excited about the CMS interoperability rule, which was delayed due to the coronavirus pandemic and has since been delayed again by the change in presidential administrations.
While many payers have opposed the CMS interoperability rule, SCAN Health Plan has factored this rule into its strategy for acquiring real-time data.
“SCAN Health Plan is looking to leverage the interoperability rule and APIs to accelerate data acquisition, reducing data latency and facilitating real-time analytics that drive improved outcomes,” Goode said.
To Goode, anything that is facilitating data exchange is a step in the right direction.
Real-time data must be a healthcare community-wide effort because a delay in data transfer in one corner of the industry can lead to delays across the chain of data exchange.
“You have to have the technology infrastructures to leverage real-time data across the board,” Goode emphasized. “What we see is that even though we get claims data real-time out of our Core-Admin system, we're still getting that claim in a lag. That claim may come to us 10, 14 days after the encounter occurred so it diminishes the value of us getting it real-time out of our Core-Admin system.”
Real-time predictive analytics requires partnerships outside of the healthcare community, as well. Woolston noted that the legal implications of predictive analytics demand that payers receive feedback from the legal community on their real-time data collection efforts.
“We partner closely with our legal and compliance teams to ensure our use, collection, or acquisition of data is in compliance with all applicable laws,” he noted.
What the future holds for real-time predictive modeling
It will be a marathon—not a sprint—to achieve PwC’s vision of an interoperable, real-time database that can inform healthcare professionals’ decision-making with zip-code level accuracy, Singh acknowledged.
Consumers will be one of the primary forces driving these changes. This has been true for the adoption of virtual care and for the development of care coordination.
“It's not just technology. It's about creating the right community, services, and capability around consumers so they make it easier,” Singh said.
SCAN Health Plan intends to expand on its interoperable functions going forward.
“You really want to be focused in on 'where are we going to really be able to move the needle with our predictive analytics?’” Goode explained.
By asking this question and paying attention to how data can best be utilized in the consumer’s favor, payers can enhance not only their real-time data analytics but also their more traditional predictive analytics processes, bolstering their forecasting abilities overall.
Aetna intends to expand on real-time data collection efforts related to internal and plan sponsor data, social determinants of health data, and vendor-provided data.
“Most importantly, we are interested in deepening our partnerships with our members and their healthcare providers, including the ability to use electronic medical record data more broadly,” added Woolston. “This would enable greater clinical specificity as well as a more powerful statistical portrait of our members when helping them on their path to better health.”
