2017 ACA Open Enrollment Data Shows 12.2M Marketplace Signups
The latest Open Enrollment Period data breaks down consumer selections, demographics, as well as state-by-state enrollment numbers.
Source: Thinkstock
- During the 2017 ACA Open Enrollment Period (OEP), more than 12.2 million healthcare consumers purchased or renewed insurance through Healthcare.gov or their local state exchanges, said CMS in a new data brief.
Marketplace consumers either selected, or were automatically re-enrolled in, a Marketplace plan throughout the 50 states and D.C. One-third of enrollees were new to the Marketplace, while half were returning customers and 18 percent were automatic re-enrollments.
Through Healthcare.gov, 74 percent of consumers in the 2017 OEP enrolled or re-enrolled in silver plans, which was an increase from 71 percent the year before.
During the enrollment period, a majority of enrollees bought health insurance by the January 1st deadline as more people sought health insurance either through state-based marketplaces or Healthcare.gov. CMS gathered the OEP data from enrollees who self-reported household income, race, rural location through Healthcare.gov and state options.
A large portion of these enrollees required financial assistance either through a premium tax credit (APTC) or cost sharing reductions (CSRs). Those who used APTC for financial assistance represented 83 percent of the new 2017 enrollees, equating to more than 10.1 million individuals. Fifty-eight percent of enrollees required CSR assistance, which is equal to another 7,050,298 people.
During the 2017 OEP, 71 percent (8,691,150 individuals) selected Silver-tier plans. Bronze plans were the second largest selection with 23 percent, while Platinum, Gold, and Catastrophic plans combined for 6 percent of enrollee selections.
Healthcare customers in the 35-54 age range (37 percent of consumers) and the 0-34 range (36 percent) comprised most of the consumer base. Only 28 percent of purchasers were aged 55 or above.
Women enrolled at a higher rate than men, with 4.9 million women (54 percent) versus 4.2 million male consumers (46 percent.). Notably, non-rural enrollees were substantially higher than rural ones. Of the Healthcare.gov users, 82 percent were non-rural and 18 percent lived in rural areas of the country.
There are notable disparities both racially and ethnically between the online enrollment groups.
A sizeable amount of Healthcare.gov selections were from whites at 48 percent, or 4.4 million people. Enrollees who did not identify their race made up 36 percent. African Americans (7 percent), Asians (7 percent), and multiracial applicants (2 percent) did not make up more than a million healthcare.gov enrollees.
In total, 71 percent of enrollees had incomes between 100 and 250 percent of the Federal Poverty Level (FPL). Enrollees who reported incomes between 251 and 400 percent of the FLP made up 17 percent of the total. The remaining 12 percent either had incomes above 400 percent or below 100 percent of the FLP.
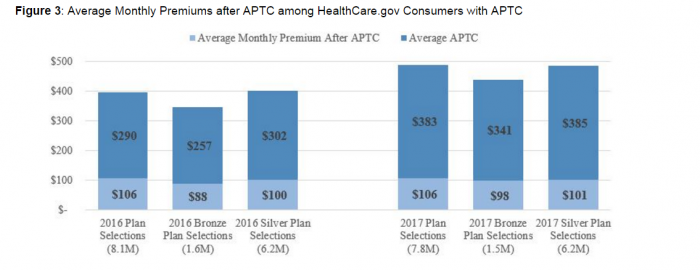
Source: Centers for Medicare and Medicaid Services
On average, the 2017 monthly APTC increased to $383 compared to $290 in 2016. However, premium prices rose from an average 2016 premium of $396/month to a 2017 premium average of$489/month.
Qualifying consumers who purchased silver plans, the most popular option ins 2017, receive APTC assistance of $385. These silver plan holders pay $101 of the $486, which rounds out to 20 percent. Silver plan holders with APTCs account for 6.2 million 2017 plan selections.
The data indicates that there is high consumer demand for Marketplace plans, as evidenced by the large enrollment numbers. Despite current political uncertainty around the future of health insurance regulations, the Marketplace appeared to offer attractive options for millions of patients on the lower end of the socioeconomic scale.
