25% of Health Plans Implement Alternative Payment Models
Multiple studies are showing that alternative payment models are becoming more common among health plans.

- Among commercial health plans, Medicare Advantage, and Medicaid markets, approximately 25 percent of reimbursement is expected to be in the form of alternative payment models by the end of 2016, according to a new report from the Health Care Payment Learning & Action Network (LAN).

The research looks at both public and private health plans in one of the most comprehensive and largest studies of this kind. The study began on May 19, 2016 and lasted until July 13, 2016, according to a press release from the Health Care Payment Learning & Action Network. More than 70 health plans participated in the study, showing the costs of medical care in 2015.
“Conducting the study has been a critically important first step in gauging the nation’s collective progress toward the adoption of APMs,” Sam Nussbaum, chair of the LAN’s APM Framework & Progress Tracking Work Group, said in the press release. “The results provide an essential benchmark for future measurement efforts. We hope the collection process coupled with the analytics to determine what is working will accelerate the transformation to value-based payment.”
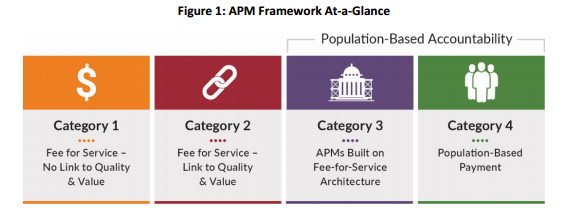
The study also points at the need for more innovation and reform in healthcare payments in order to financially incentivize providers and hospitals to improve quality and bring more value to the patient community. The researchers from LAN defined alternative payment models using several categories. The first category outlines fee-for-service and is not tied to quality or value.
Three other categories include (1) fee-for-service linked to quality and value, (2) alternative payment models based on fee-for-service building blocks, and (3) population-based payment systems.
The results from the surveys used in the study show that, in 2015, 62 percent of healthcare dollars were still spent in the fee-for-service category not tied to value or quality. However, this means that a solid 38 percent of healthcare dollars were spent in a value-based care reimbursement model last year. Out of all health plans surveyed, 15 percent of healthcare dollars were in the form of fee-for-service linked to value while 23 percent were in either alternative payment models or population-based reimbursement systems.
“This report shows the meaningful progress we’ve made to improve quality and lower costs,” said Marilyn Tavenner, President and CEO of America’s Health Insurance Plans. “Health plans, doctors, hospitals, businesses, and public programs are all changing, all collaborating – and all improving the way we deliver care. We’re being smarter purchasers of health care by prioritizing efficient, effective, and evidence-based approaches to delivering care. That means better quality for patients and lower costs for consumers.”
When looking at the 2016 year, the rate of healthcare dollars in the third and fourth categories increased to 25 percent with 41 percent of this rise seen in the Medicare Advantage market. This shows that alternative payment models are steadily becoming more popular in the health insurance market especially within Medicare.
“I’m excited to see that almost 25 percent of payments nationally are in APMs supporting better care, smarter spending, and healthier people,” Patrick Conway, Chief Medical Officer for the Centers for Medicare & Medicaid Services (CMS) and Director of the Center for Medicare & Medicaid Innovation, said in a public statement. “CMS now wants to work with the private sector to reach our goal of 50% of payments in these models by the end of 2018.”
LAN has set out a goal of bringing at least 30 percent of total US healthcare spending toward alternative payment models by the end of 2016. The results from the study seem promising.
The healthcare industry has been steadily moving toward adopting value-based care and alternative payment models in recent years. One report conducted by ORC International and commissioned by McKesson shows that 58 percent of polled payers are on their way toward adopting value-based care reimbursement platforms.
The rate found in this survey rose by 10 percent from 2014, which shows how alternative payment models are becoming more common around the nation. Additionally, the polled payers predicted that at least 60 percent of their reimbursement contracts will likely be based on value over the next five years.
The results showed that value-based care reimbursement like bundled payments would rise in popularity with those polled predicting a 6 percent rise in bundles over the next five years. However, more preparation may be needed as only half of the polled payers and 40 percent of surveyed providers stated being ready to adopt bundled payment models.
Higher adoption rates of alternative payment models or value-based care may be due to healthcare legislation like the Affordable Care Act and the creation of health insurance exchanges, said Kevin Counihan, CEO of the Health Insurance Marketplace. Essentially, the exchanges are a place where payers can redesign their health plans in a way to decrease healthcare spending.
Health payers that haven’t invested resources in adopting alternative payment models at this point may need to join the movement toward value-based care reimbursement before they fall behind any further.
Image Credits: Health Care Payment Learning & Action Network
Dig Deeper:
How to Overcome the Challenges of Bundled Payment Models
Private Payers Follow CMS Lead, Adopt Value-Based Care Payment