4 Elements Necessary for Switching to ICD-10 Diagnosis Coding
CMS offered end-to-end testing for a number of providers in order to ensure the industry was ready to switch to ICD-10 diagnosis coding.

- On October 1, 2015, the healthcare industry from payers and federal agencies to hospitals, physicians, and specialists transitioned to ICD-10 diagnosis coding. Many healthcare providers were concerned that their practices would not be prepared to transition to the more complex ICD-10 diagnosis coding set, but the Centers for Medicare & Medicaid Services (CMS) had spent several years preparing the industry for this major change.
CMS Acting Administrator Andy Slavitt wrote for the CMS Blog about the major transition to ICD-10 diagnosis coding. Slavitt compared it to the Y2K of healthcare since, if not implemented correctly, it could create havoc among hospitals, clinics, and insurers.
Many thought that physicians from rural communities would have difficulty preparing and meeting the October 1 ICD-10 transition deadline. CMS has been responsible for getting payers and providers through some of the most complex implementations including the Affordable Care Act’s health insurance exchange and the ICD-10 diagnosis coding transition.
The customer-centric approach
Slavitt described the four elements that CMS follows when implementing a huge project like the ICD-10 transition. First, it is vital to focus on the customer when beginning any new project or developing a program.
It was important for CMS to listen to the issues that doctors face every day when utilizing diagnostic codes and documenting clinical visits. CMS also provided training videos to help transition insurance companies, clearinghouses, hospitals, and medical practices to the new ICD-10 codes.
Also, a Road to 10 website offered some useful tips and advice to providers with regard to integrating new ICD-10 systems and protocols. Most importantly, CMS offered end-to-end testing for a number of providers in order to ensure the industry was ready to switch to ICD-10 diagnosis coding.
Collaboration is key
Slavitt explains that CMS is dedicated to collaborating with the healthcare community when adopting new processes and making major changes. CMS worked with a number of important physician groups when transitioning the healthcare industry to the ICD-10 coding set including the American Hospital Association, the American Medical Association, and the American Health Information Management Association.
The Acting Administrator mentions that CMS worked with stakeholders and collaborated on major and minor issues in order to ensure the ICD-10 transition was successful. Physician concerns were addressed and assistance was offered.
Remain responsive
The healthcare system often encounters challenges, but CMS remains accountable for any problems and works to address and solve issues, Slavitt explained. Hospitals, health plans, and doctors’ offices were all at risk of potential issues during the ICD-10 transition and CMS committed to resolving all issues within three business days.
After the October 1 deadline, CMS received about 1,000 inquiries regarding some obstacles with filing ICD-10 claims. The organization was able to respond to 100 percent of these issues within three business days, as promised.
Utilize metrics and analytics
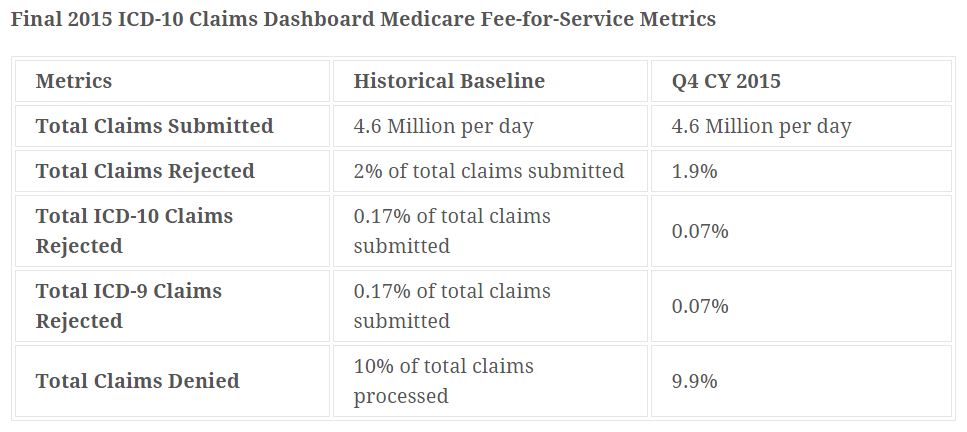
Slavitt mentioned that using scorecards and daily spreadsheets will keep any big project in check. After October 1, it was vital for CMS to track which providers were sending claims, the rates of claim processing, and if any hospitals or physician practices were having difficulty sending claims. When it comes to claim denial or any issues in certain states, CMS needed to know as soon as possible to fix any problems.
As such, metrics and analytics was vital to the ICD-10 transition. A scorecard and heat map was used to track these metrics. Additionally, an ICD-10 Coordination Center was created to handle any problems that arose after the implementation deadline. The results speak for themselves. The ICD-10 transition was a relative success for CMS and healthcare providers around the nation.
“For thousands of physicians and other clinicians around the country, the change to ICD-10 was a big undertaking, requiring time, planning, and a period of adjustment,” Slavitt wrote. “But on October 1, proper execution and good implementation made all the difference. On the big day, the ICD-10 Coordination Center was packed, and the CMS teams and our partners were geared up and ready to make sure that any burden on physicians could be minimized and concerns quickly addressed.”
At the end of October 2015, CMS was reporting that claims processing had been going smoothly after the ICD-10 implementation deadline passed. At the time, out of 4.6 million claims submitted daily, only 0.09 percent were rejected due to ICD-10 coding failures. In addition to the ICD-10 coding issues, 0.11 percent of claims were rejected because of misuse of ICD-9 codes.
“No one is in a position yet where they can just assume they have this down and can just go about their business. They have to keep analyzing the data and finding out what's causing the denials and then provide education,” Dave McCann, Managing Director at Berkeley Research Group’s Clinical Economics practice, told RevCycleIntelligence.com.
Nonetheless, there are many positives associated with switching to the ICD-10 diagnosis coding set and the Coalition for ICD-10 presented their case in a release on October 1.
“As a result of the replacement of the obsolete ICD-9-CM with the more modern ICD-10-CM and ICD-10-PCS code sets, patients can look forward to complete, accurate, up-to-date diagnostic and procedural data necessary to achieve significant advances in the quality of care and more efficient healthcare administrative processes,” the Coalition for ICD-10 stated.
“The Coalition for ICD-10 is very pleased that the U.S. healthcare industry can finally begin to leverage the many opportunities anticipated by the availability of better healthcare data – including improved patient outcomes, patient safety, and population health, lower healthcare costs, and adoption of new payment models that reward value.”
Image Credits: Centers for Medicare & Medicaid Services