Accountable Care Organizations Keep Growing Across US
Why is it that accountable care organizations have been proliferating at such great speed around the nation?

- The Patient Protection and Affordable Care Act led to the development of the Medicare and Medicaid Innovation Center, which eventually brought the creation of accountable care organizations and the Medicare Shared Savings Program. Over the last several years, the number of accountable care organizations has grown tremendously around the country.

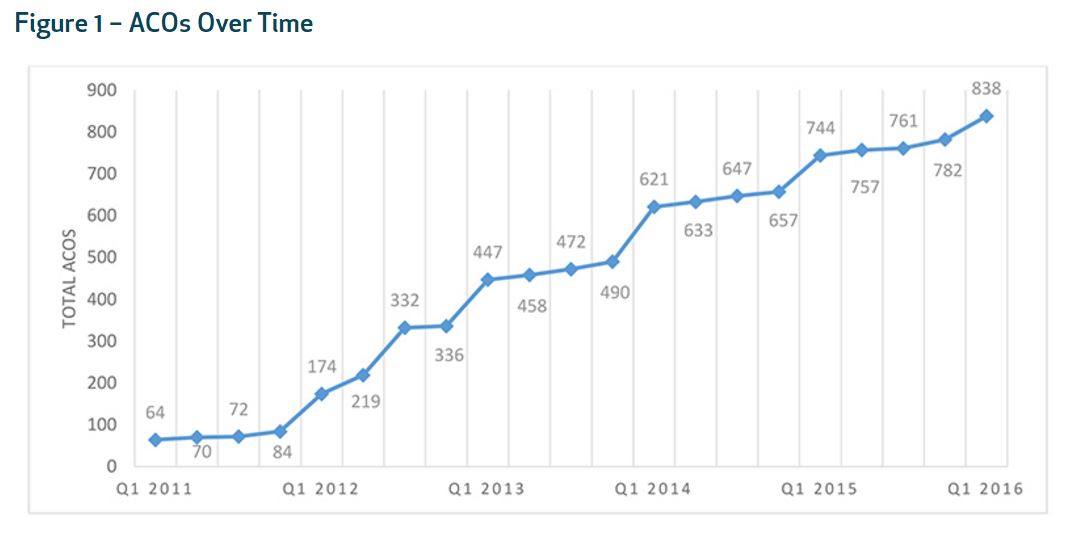
Leavitt Partners along with the Accountable Care Learning Collaborative conducted a study in January 2016, as reported by the Health Affairs Blog, that found a total of 838 accountable care organizations across all 50 states in the nation. In fact, the number of accountable care organizations has grown by 12.6 percent in just the last year.
In addition to these findings, there is currently more than 1,200 accountable care contracts being implemented across hospitals throughout the US. The study discovered that 28.3 million patients are now receiving medical services through an accountable care organization or ACO.
The Medicare Shared Savings Program is now on its third year and many ACOs have renewed their contracts while several have decided to forego another year performing under the accountable care contract.
“One important indication of the success of the early ACO initiatives is how many renew their contracts when they have the option of leaving an accountable care program,” the report stated.
“Of the 220 Medicare ACOs that were eligible for renewal, 147 renewed in the MSSP, eight transitioned to the Next Generation ACO program, and an additional 10 combined or merged with other ACOs. Collectively, three-fourths of the early Medicare ACOs are continuing onward with a Medicare ACO program. In addition, a number of those that have left the Medicare program continue to have commercial ACO contracts, indicating that ACO policy refinements may further increase participation.”
“Fully adopting accountable care and successfully transforming a practice to achieve savings is difficult, with mixed results among participants. Many ACOs have not succeeded, and it is likely that more ACOs will ultimately be unsuccessful at making this transition. Other ACOs will likely drop out of government and commercial contracts in the future.”
“But knowledge about how to succeed as an ACO will continue to increase, and organizations that dropped out will have the opportunity to try again in the future in modified ACO programs. Thus, many organizations will iterate as they learn how to make their transition to accountable care.”
The study also shows that states who have adopted Medicaid accountable care organizations tend to have a higher percentage of patients covered under the ACO model of care. The report finds that the number of ACOs countrywide has grown steadily since 2011.
Why is it that accountable care organizations have been proliferating at such great speed around the nation? Part of the reason may be due to the fact that the federal government and the health insurance industry is attempting to move hospitals and medical facilities away from utilizing the fee-for-service payment model and embracing value-based care reimbursement.
The report further discusses the new policies that the Department of Health and Human Services (HHS) has begun adopting. For example, HHS expects 50 percent of Medicare payments to be in the form of alternative payment models by the end of 2018. Currently, 30 percent of Medicare payments have already been positioned in a value-based care reimbursement model.
In order to gain greater success, accountable care organizations have begun embracing value-based care reimbursement, which includes meeting quality metrics and reducing healthcare spending. The Centers for Medicare & Medicaid Services (CMS) have continually stressed value-based care and alternative payment models, which is clearly seen within the new MACRA legislation.
Leadership skills have also been an important aspect of running a successful accountable care organization as well as trust and care coordination between partnering hospitals or medical facilities. Health payers will need to work with ACOs to improve communication and ensure clear understanding between facilities.
Essentially, accountable care organizations have been proliferating throughout the country and some have shown real benefit to patient care along with a stabilization in healthcare spending. For instance, the Anthem Blue Cross accountable care organization (ACO) has shown a savings of $14.8 million during the 2013 to 2014 years.
The Anthem Blue Cross ACO showed a clear diversion from the fee-for-service payment system as the use of many medical services actually fell significantly. For instance, inpatient admissions fell by 5.1 percent and outpatient visits decreased by 7.5 percent.
The overuse of medical services which often leads to wasteful healthcare spending seems to be decreasing in an accountable care environment. However, healthcare payers and providers will need to ensure that patient care and necessary services are not under-used in a value-based care reimbursement model.
In essence, the health insurance industry is likely to see significant benefits from accountable care organizations as these new healthcare delivery and payment systems are capable of saving significant costs and cutting wasteful spending.
Dig Deeper:
Payers Continue Favoring Accountable Care Organizations
Physician Leadership Key to Accountable Care Organizations