AMA: Payers Moving Too Slowly on Prior Authorization Fixes
Payers are not working quickly enough to address significant burdens associated with prior authorizations, the AMA asserts.

Source: Thinkstock
- Physicians are still frustrated by problematic prior authorization (PA) procedures and believe that health payers are moving too slowly on necessary solutions, finds a new survey by the American Medical Association (AMA).
Building on data released earlier in 2019, which showed near-universal dissatisfaction with PA protocols, the AMA is again urging health plans to reduce the administrative burdens associated with the pre-approval process.
“While health plans and benefit managers contend that PA programs are important to control costs, providers often find these programs to be burdensome and barriers to the delivery of necessary patient care,” the professional organization wrote.
To combat perceptions of burden while maintaining the benefits of PA for controlling costs, the AMA collaborated with other major industry groups to develop a framework for using PAs effectively.
The American Hospital Association, AHIP, Blue Cross Blue Shield Association, MGMA, and the American Pharmacists Association all signed off on the 2018 Consensus Statement on Improving the Prior Authorization Process.
READ MORE: CAQH CORE Urges Industry Collaboration on Prior Authorizations
Yet the AMA believes that industry stakeholders are not moving quickly enough to address the shared areas of concern, such as targeting PAs to specific situations, embracing automation, and improving transparency and communication around the PA process.
A survey of 1000 practicing physicians confirms the group’s concerns, the AMA contends.
For example, payers signing the industry consensus statement agreed to address communication barriers and encourage the adoption of automated, digital techniques for sending and receiving PA information.
“Moving toward industry-wide adoption of electronic prior authorization transactions based on existing national standards has the potential to streamline and improve the process for all stakeholders,” the statement says.
“Additionally, making prior authorization requirements and other formulary information electronically accessible to health care providers at the point-of-care in EHRs and pharmacy systems will improve process efficiencies, reduce time to treatment, and potentially result in fewer prior authorization requests because health care providers will have the coverage information they need when making treatment decisions.”
READ MORE: 91% of Physicians Say Prior Authorizations Negatively Impact Care
However, 69 percent of survey participants said that it is still somewhat or extremely difficult to communicate with payers around prior authorizations. Physicians find it challenging to determine what services or prescriptions require a PA and what criteria support the decision.
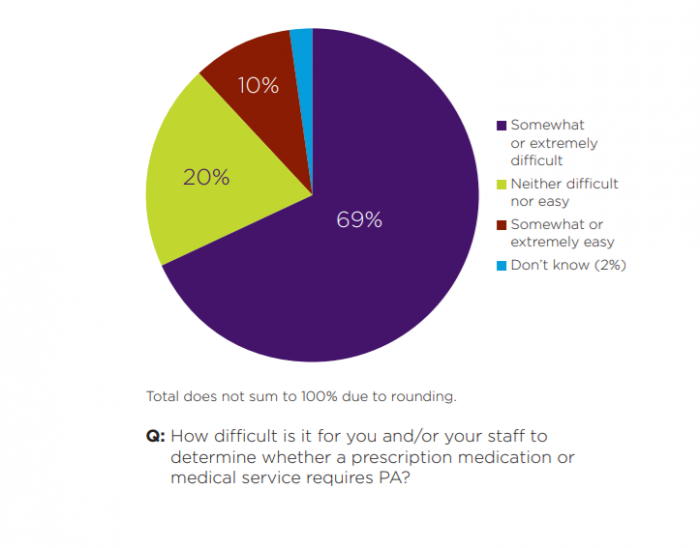
Source: AMA
In addition, few physicians are able to conduct PA transactions through modern digital means. Only 21 percent of providers reported that their electronic health record (EHR) systems are able to support electronic PA for prescription drugs.
About 60 percent of physicians commonly use the phone for PAs related to prescriptions and medical services. Nearly half of physicians routinely use fax machines for the process.
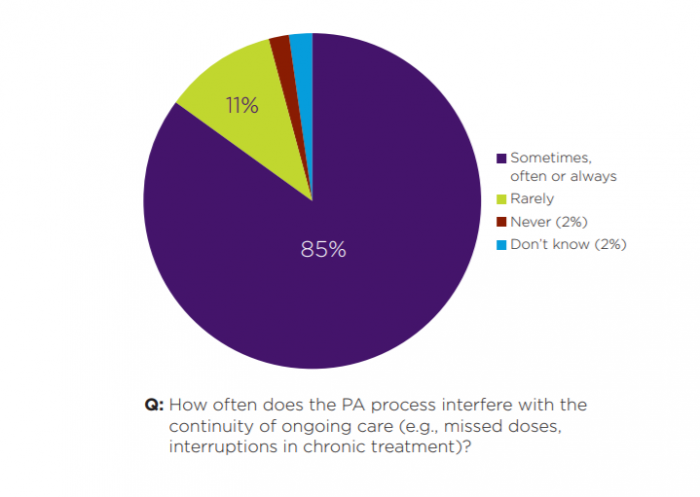
As a result of slow and unwieldy communication processes, physicians report that the continuity of care for their patients is frequently interrupted.
Eighty-five percent of respondents said that PAs sometimes, often, or always interfere with the continuity of care by introducing delays or detours in treatment.
READ MORE: 96% of Payers Are Committed to Electronic Prior Authorization
In the earlier survey, 91 percent of physicians also stated that prior authorizations actively contribute to worse outcomes for patients. Patients are more likely to abandon treatment or experience delays in necessary care when PAs are involved, they asserted.
About two-thirds of physicians wait at least one business day for a response to a PA request. A quarter routinely wait more than three days.
The industry has also pledged to address these inefficiencies by developing more selective PA criteria.
“Differentiating the application of prior authorization based on provider performance on quality measures and adherence to evidence-based medicine or other contractual agreements (i.e., risk-sharing arrangements) can be helpful in targeting prior authorization requirements where they are needed most and reducing the administrative burden on health care providers,” the consensus statement says.
“Criteria for selective application of prior authorization requirements may include, for example, ordering/prescribing patterns that align with evidence-based guidelines and historically high prior authorization approval rates.”
But only 8 percent of physicians reported contracting with health plans that allow exemptions for providers, the AMA says.
Source: AMA
Instead of narrowing the focus and reducing the number of required PAs, payers are actually on the opposite path, the survey indicates.
Eighty-six percent of respondents have seen increases in PAs for medical services and 88 have seen more prescription PAs over the past five years, the poll found.
However, since the industry consensus statement was only signed in 2018, this statistic may not be a useful assessment of progress since the agreement.
Nevertheless, physicians are united in their view that the prior authorization process is ripe for change, and the AMA is clearly strongly invested in pushing speedier progress.
The society has published an extensive list of reports, recommendations, and principles related to member concerns about PAs, and offers providers a number of resources to help physicians understand and navigate the process.
“The AMA is committed to attacking the dysfunction in health care by removing the obstacles and burdens that interfere with patient care,” said AMA Board of Trustees Chair Jack Resneck Jr., MD, after the release of the first survey data in February.
“To make the patient-physician relationship more valued than paperwork, the AMA has taken a leading role by creating collaborative solutions to right-size and streamline prior authorization and help patients access safe, timely and affordable care, while reducing administrative burdens that pull physicians away from patient care.”
“The time is now for insurance companies to work with physicians, not against us, to improve and streamline the prior authorization process so that patients are ensured timely access to the evidence-based, quality health care they need.”
