Challenges, Advantages of Merit-Based Incentive Payment System
While the Merit-Based Incentive Payment System clearly has benefits for the Medicare program, there are substantial challenges standing in the way of this program.

- The Merit-Based Incentive Payment System (MIPS) is a new reimbursement program used by the Centers for Medicare & Medicaid Services (CMS) that has its own unique set of challenges and advantages for provider payment.

Earlier this year, the federal government passed a law called the Medicare Access & CHIP Reauthorization Act of 2015 (MACRA), which repealed the Sustainable Growth Rate (SGR) formula. This has dramatically transformed the way Medicare pays providers for Medicare services.
CMS reports that the SGR formula will no longer be used to determine Medicare payments. Additionally, MACRA establishes a strong framework in which providers will be compensated based on quality care instead of merely greater quantity of services. Additionally, MACRA allows CMS to combine its several quality reporting programs into one encompassing system.
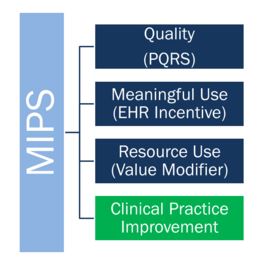
This is where the Merit-Based Incentive Payment System comes in. MIPS incorporates the Physician Quality Reporting System, the Value-based Payment Modifier, and the Medicare EHR Incentive Program all into one general model of reimbursement.
While the Merit-Based Incentive Payment System clearly has benefits for the Medicare program, there are substantial challenges standing in the way of this program.
Challenge 1: Lack of incentives
The Medicare Payment Advisory Commission sent a letter to Andrew Slavitt, the Acting Administrator of CMS, outlining the lack of incentives for providers taking part in the Merit-Based Incentive Payment System.
While providers who take part in Alternative Payment Models will be eligible to receive financial incentives from 2019 to 2024, those taking part in MIPS or fee-for-service reimbursement models would not be receiving any such bonuses and would receive lower reimbursement rates that those taking part in alternative payments starting in 2025.
Advantage 1: Stronger benchmarks and pull for alternative payment models
According to the New England Journal of Medicine, the new policies under MACRA are providing greater incentive for physicians to participate in alternative payment models. CMS is even looking to push forward bundled payments and require its use among joint replacement surgeries. MIPS and Alternative Payment Models bring more strict benchmarks for providers to follow in improving the quality of care across their facilities.
“The recently passed Medicare Access and CHIP Reauthorization Act (MACRA), which replaced the SGR with a Merit-Based Incentive Payment System (MIPS), opens the way for better benchmarks by providing a strong incentive for physicians to participate in APMs,” the paper stated. “Where evidence of their effectiveness is strong, bundled payments can be mandated. The recent proposal by Medicare to mandate bundled payment for joint replacement and transition to a regional benchmark is encouraging.”
Challenge 2: Flaws in aligning stakeholders
Quality measures under alternative reimbursement programs and the Merit-Based Incentive Payment System like Physician Quality Reporting will need to be more simplified while quality data needs to be in user-friendly form in order to truly benefit beneficiaries. The more complex documentation standards are bringing difficulty in helping align beneficiaries among the payers and providers.
There is also a lack of alignment between Medicare, Medicaid programs, and commercial payers when it comes to quality measures. This has led to significant burden among providers when it comes to improving performance. More discussion is needed among payers, providers, healthcare associations, and quality-measurement professionals in order to reduce this lack of alignment.
Advantage 2: MIPS advances healthcare reform
The American College of Cardiology stated on its website that MIPS will consist of three already existing programs – Physician Quality Reporting System, Meaningful Use, and the Value-based Payment Modifier – along with a new Clinical Practice Improvement category.
Clinical Practice Improvement will essentially reward those providers who are working toward implementing healthcare reform strategies such as greater care coordination and a focus on patient safety. This may include the use of telehealth technology or taking part in a patient-centered home as well as clinical data registry.
“The clinical practice improvement category will recognize clinicians for activities that contribute to advancing patient care, safety and care coordination,” the American College of Cardiology stated.
Challenge 3: Lack of consumer engagement measures
It seems that MACRA has not led to the creation of Medicare Alternative Payment Models that support the work of providers in boosting patient and consumer engagement. The measures under alternative reimbursement strategies do not push forward greater focus on patient engagement, according to the New England Journal of Medicine.
When it comes to chronic disease management, patient engagement is vital in order to ensure the right medications are taken at the right time, patients stick to their appointments, and a healthy lifestyle is incorporated throughout the consumer base. It is beneficial for future quality measurement programs to incorporate patient engagement benchmarks in order to truly improve health outcomes.
Advantage 3: Focus on value-based care cuts costs
The Commonwealth Fund outlines how repealing the SGR formula will likely bring healthcare providers to adopt alternative payment models and value-based care while leaving fee-for-service payment models in the past.
Greater focus on value-based care will also lead to the reduction in unnecessary procedures and wasteful spending, as providers will be focused on quality instead of quantity. This should lead to lower medical costs overall.
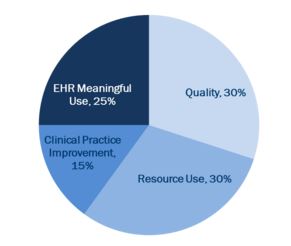
“To accelerate the move from volume-based to value-based payment, a merit-based incentive payment system (MIPS) will be established beginning in 2019,” The Commonwealth Fund reports. “The MIPS will replace three previous incentive programs with a combined value-based payment program that assesses the performance of each eligible provider based on quality, resource use, clinical practice improvement activities, and meaningful use of certified electronic health record technology.”