CMS Continues to Reform through Healthcare Bundled Payments
In order to implement healthcare bundled payments, providers need to be prepared to negotiate a risk-based contract.

- As of April 1, 2016, healthcare bundled payments have become a part of the reimbursement strategy of hospitals providing hip and knee replacement surgeries as well as the Centers for Medicare & Medicaid Services (CMS) itself. Through the Comprehensive Care for Joint Replacement (CJR) model, CMS is using healthcare bundled payments to reimburse for an episode of care and, thereby, improve patient health outcomes and work toward reducing medical spending.

“This model is about improving patient care. Patients want high quality, coordinated care – not just for a day, but for an entire episode of care. Hospitals, physicians, and other providers who work together can be successful and improve care for patients in this model, and CMS will help providers succeed,” Patrick Conway, M.D., CMS’ Principal Deputy Administrator and Chief Medical Officer, said in a public statement.
When looking at a mere two years ago, the numbers of Medicare beneficiaries receiving joint replacement surgeries hit more than 400,000 and cost hospitals over $7 billion. The issue at hand has been the variance in the quality and cost of hip or knee replacement surgeries among multiple providers. The Comprehensive Care for Joint Replacement model and healthcare bundled payments are meant to bring hospitals onto the same level of high quality care and spending.
Essentially, CMS is looking to improve the care coordination between hospitals, skilled nursing facilities, rehabilitation centers, and home health agencies through a reimbursement structure that focuses on an episode of care instead of individual services.
This model is being implemented in hospitals across 67 metropolitan areas and, based on public stakeholder comments, CMS has created more incentives and performance measure scoring within this program to stimulate hospitals toward improving quality of care and patient health outcomes. When designing the Comprehensive Care for Joint Replacement program, CMS followed the examples set forth for healthcare bundled payments from the private sector.
 “We are embarking on one of the most important steps we will take to improve the quality and value of care for hundreds of thousands of Americans who have hip and knee replacements through Medicare every year,” Health and Human Services Secretary Sylvia M. Burwell stated in a press release. “By focusing on episodes of care, rather than a piecemeal system, we provide hospitals and physicians an incentive to work together to deliver the best care possible to patients.”
“We are embarking on one of the most important steps we will take to improve the quality and value of care for hundreds of thousands of Americans who have hip and knee replacements through Medicare every year,” Health and Human Services Secretary Sylvia M. Burwell stated in a press release. “By focusing on episodes of care, rather than a piecemeal system, we provide hospitals and physicians an incentive to work together to deliver the best care possible to patients.”
The American Medical Association (AMA) explains how healthcare bundled payments work, which is by providing a single payment to a hospital or other medical facility for an episode of care instead of individual fees paid out to surgeons, anesthesiologists, nurses, and rehabilitation staff.
Sometimes an accountable care organization operates through bundles and may receive one lump sum that is then divided amongst each provider. Other times, payers will reimburse each provider individually for all services performed in a specified period of time.
In order to implement healthcare bundled payments, providers need to be prepared to negotiate a risk-based contract. For instance, if medical services, treatments, and other complications actually end up being more expensive than the agreed upon price in the bundled payment contract, providers would need to cover those costs themselves. However, if providers are able to spend less funds on treating a patient than the contract dictates, they are free to keep the difference.
In a health policy brief released by the Robert Wood Johnson Foundation, recent healthcare payment reforms as presented by CMS were discussed. When the Affordable Care Act was passed, CMS gained greater authority in reforming the reimbursement structures among hospitals and Medicare/Medicaid programs.
The Secretary of the Department of Health and Human Services (HHS), Sylvia M. Burwell, has required for 50 percent of Medicare payments made out to providers to be in the form alternative payment models by the end of 2018. This shows how important bundled payments and value-based care reimbursement is for the federal government and the health insurance industry as well.
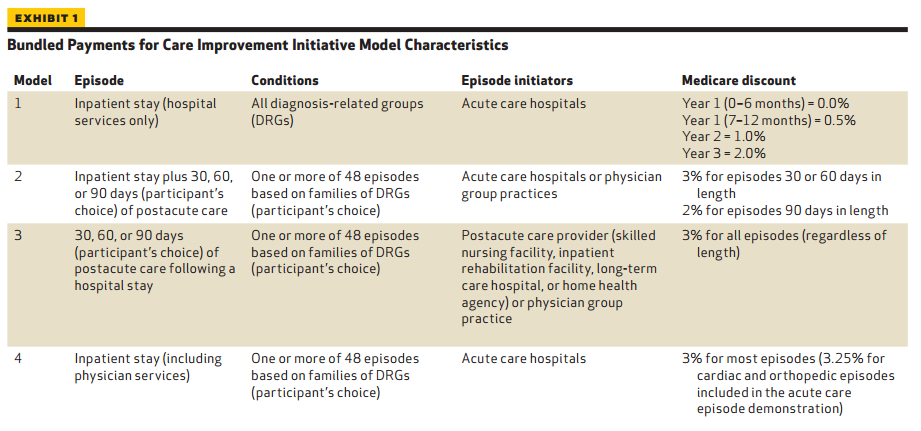
The Bundled Payments for Care Improvement (BPCI) is another program developed by CMS to push forward healthcare bundled payments. Four different models are being tested in this program and each includes reimbursement for a hospital inpatient stay.
While the first model is focused specifically on the medical care received during the hospital stay, the other three are more geared toward post-acute care after discharge. Once again, CMS is aiming at improving care coordination and boosting health outcomes by implementing healthcare bundled payments. The hopes for the program include reducing wasteful spending and other inefficiencies throughout the healthcare delivery system.
“The ultimate aim of the BPCI initiative is to not just change how Medicare pays for services but to prompt changes in how health care is delivered in the United States,” the health policy brief stated.
“Medicare’s participation is critical to this goal: Other payers are also experimenting with bundled payments, but as a national program with more than forty-five million beneficiaries, Medicare is a primary driving force behind change in the health care arena. Therefore, the design and structure of the BPCI initiative are particularly important as they will likely influence how other payers approach episode-based payments.”
“CMS has identified multiple goals for the BPCI initiative including the following: aligning Medicare payment with how patients experience care, supporting and encouraging providers interested in redesigning care, and providing as much flexibility as possible for providers to redesign care to meet the needs of their specific community.”
Whether it is through the Comprehensive Care for Joint Replacement (CJR) model or the Bundled Payments for Care Improvement (BPCI) program, the federal agency is aiming its sights on reforming reimbursement throughout the healthcare industry, reducing medical spending, and strengthening the quality of care.
Image Credits: Robert Wood Johnson Foundation