HHS Cites Affordable Care Act Led to Prescription Drug Savings
The Affordable Care Act seeks ways to make both prescription drug coverage and preventive services more cost-effective for consumers.

- Yesterday the Department of Health and Human Services (HHS) announced that millions of Medicare beneficiaries continue to see benefits from the Affordable Care Act especially with regard to their savings with prescription drugs. Approximately 10.7 million elderly beneficiaries have received discounts on prescription drugs, which amounts to $20.8 billion in savings or almost $2,000 per Medicare beneficiary.

These cost savings in prescription drug coverage have come about ever since the Affordable Care Act was established, according to the Centers for Medicare & Medicaid Services (CMS). The results show that, in 2015, $5.4 billion in discounts were offered to 5.2 million seniors and people with disabilities under the Medicare program, which amounted to $1,054 per beneficiary.
This was a steady increase from the prescription drug saving results found in 2014, CMS reported. In addition to the discounts on prescription drugs, Medicare beneficiaries are also benefiting from preventive medical services offered without out-of-pocket expenses or coinsurance costs.
39.2 million Medicare and Medicare Advantage members took part in one or more preventive service(s) without copays or deductibles in 2015, which was a minor increase from the results found in 2014. Along with these findings, about 9 million Medicare and Medicare Advantage beneficiaries took part in an annual wellness visit at their doctor’s office in 2015. When comparing these results to 2014, about one million more people chose to take advantage of annual wellness visits last year.
Due to Obamacare, annual wellness visits are now completely covered for Medicare beneficiaries without needing coinsurance or Part B deductibles for specific preventive services. These preventive medical services consist of many different types of cancer screenings among other advantages. The healthcare law helps patients, providers, and payers prevent serious illnesses, diagnose disease before significant problems arise, and monitor medical conditions.
“Medicare consumers are now more engaged and empowered in their own health thanks to the Affordable Care Act,” Centers for Medicare & Medicaid Services (CMS) Acting Administrator Andy Slavitt said in a public statement. “Millions are now able to access more affordable prescription medicine for their chronic conditions and millions more are staying healthier by accessing preventive services, especially vital for people living with disabilities or growing older.”
The Affordable Care Act seeks ways to make both prescription drug coverage and preventive services more cost-effective for consumers. In particular, the Affordable Care Act closes the prescription drug “donut hole,” which essentially means beneficiaries had to pay full price for prescribed medicine out-of-pocket “before catastrophic coverage for prescriptions took effect,” the CMS brief explained.
The gap in covering prescription drug costs among Medicare beneficiaries is known as the “donut hole” and the Affordable Care Act seeks to close the gap completely by 2020. First, in 2010, Medicare beneficiaries with a prescription drug coverage plan who fell into the “donut hole” received a rebate of $250 due to the provisions of the healthcare law.
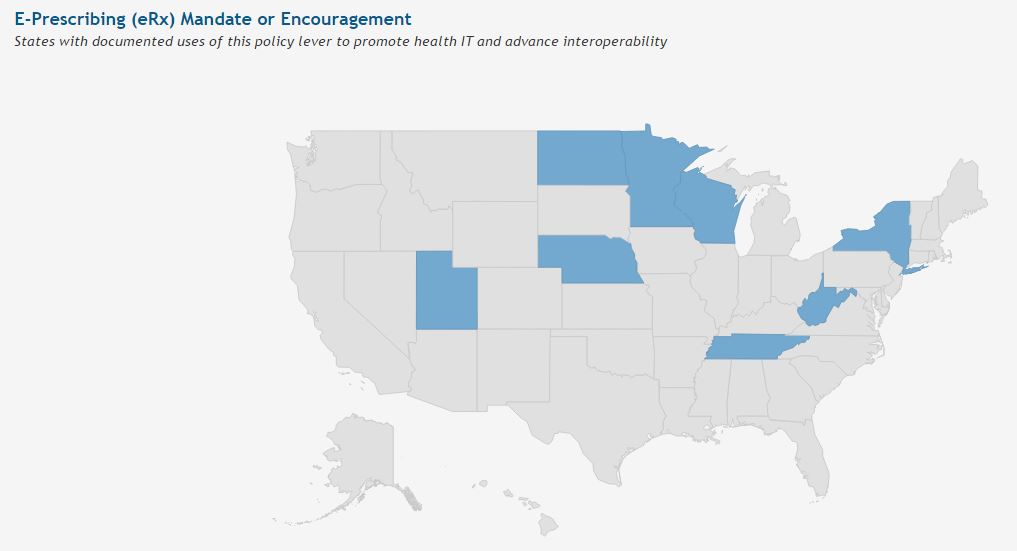
In 2011, Medicare members who fell into the “donut hole” obtained discounts and savings on brand-name and generic drugs. Medicare Part D beneficiaries within the “donut hole” will receive discounts and savings this year, which will amount to 55 percent of brand name drug costs and 42 percent of generic drug prices. CMS has also sought to increase use of technology associated with prescribing medication. Electronic prescribing requirements were positioned within the Medicare and Medicaid EHR Incentive Programs and the interoperability of e-prescribing is now slowly becoming a mainstay around the nation.
While Medicare beneficiaries may be seeing a decrease in their personal out-of-pocket expenses related to prescription drugs, the overall cost of medicine is soaring countrywide nonetheless. Dr. John R. Patrick, author of Health Attitude: Unraveling and Solving the Complexities of Healthcare, explained why this is so.
“The culprit in this area is Congress. The pharmaceutical lobby convinces Congress to do things that are not in the best interest of the American people but in the best interest of the pharmaceutical industry. For example, in Medicare Part D, the prescription drug plan put in place in 2003, Congress inserted a provision into the legislation preventing Medicare from negotiating the price for the drugs they pay,” Dr. Patrick stated. “It’s outrageous. The American people should be outraged and demand an explanation from Congress.”
“It’s a major contributor to the high cost of drugs. There’s no effective competition and they have the free hand to set prices wherever they want. Medicare pays it. Other countries do negotiate over the price. They pay a lot less than we do for exactly the same drugs.”
“For example, the price for one common pill in the US is $5.20 and it’s a $1.30 in Canada. This is the same pill made by the same company. This is because Congress doesn’t allow Medicare to negotiate and regulators do not allow Americans to buy drugs from Canada.”
While there are still improvements that need to be made in terms of prescription drug affordability, CMS is continually seeking to improve healthcare delivery through physician incentives tied to quality metrics, utilizing health data analytics to boost patient outcomes, and improving coordination and integration of medical care.
The Affordable Care Act also looks to stimulate preventive services by eliminating beneficiary cost sharing and reward physicians based on the quality of care instead of the quantity.
The federal agency also announced last year its “goal of tying 30 percent of Medicare payments to quality and value through alternative payment models by 2016 and 50 percent of payments by 2018.”
The Health Care Payment Learning and Action Network was created in order to help healthcare providers and payers work together to bring reimbursement for medical services onto a value-based care platform. At this moment in time, more than 4,600 providers, payers, patient groups, state agencies, consumer groups, and employers have used the Health Care Payment Learning and Action Network to bring the healthcare industry toward a value and quality-based reimbursement arrangement.
Due to the provisions of the Patient Protection and Affordable Care Act, Medicare beneficiaries can now benefit from lower out-of-pocket expenses for prescription drugs as well as cost-effective cancer screenings and wellness visits.
Image Credits: Office of the National Coordinator for Health IT (ONC)