How Maternity Care Home Model Reduces Premature Birth Rate
A maternity care home model is making headway at reducing the rates of preterm births.

- The healthcare industry has often found it problematic and costly to manage the health of newborns and mothers of preterm births. There have been social problems among pregnant women that have led to higher rates of preterm births such as trauma, living in environments filled with toxic stress, and undiagnosed and/or untreated mental health concerns, says Jennie Oberkrom, a Licensed Clinical Social Worker, Program Coordinator, and Behavioral Health Specialist from Signature Medical Group. However, Signature’s new maternity care home model is providing enhanced prenatal care developed through the Centers for Medicare and Medicaid Services (CMS) Strong Start for Mothers and Newborns Initiative and has improved health outcomes in this arena.

“It’s my job to really educate about how psychosocial issues impact overall health and pregnancy outcomes,” she told HealthPayerIntelligence.com. “I provide management to the other social workers and clinical expertise and case consulting as needed to all of our medical staff to help them understand how these psychosocial issues really impact health. We are an interdisciplinary team and the social workers will meet with the patients about three times throughout the pregnancy at the beginning, during the third trimester, and postpartum.”
“We are also available for crisis intervention because a lot of our moms are coming into the program with emergency needs like homelessness, chronic unemployment, inadequate food supply, or intimate partner violence, and more issues that we help to stabilize quickly,” Oberkrom continued. “We help with anything that is considered stressful that a woman or a family would experience throughout her pregnancy and 10 weeks postpartum.”
How care coordination saved the day
“We had a patient, Bridget, and she missed an appointment. I called her and I heard her moaning and groaning on the phone. It dawned on me that she might be experiencing labor. So I had our nurse navigator call and she triaged her. She was 32 weeks pregnant. We were able to have her admitted to the hospital and her preterm labor was stopped. She went on to deliver a healthy, baby boy at full term. The care coordination between the nurse navigator, the OB physicians who admitted the patient, working telephonically, and myself doing the home visiting, benefited this patient,” Oberkrom explained.
“The story behind the story is that Bridget was a caregiver for her mother who was struggling with lymphoma and was very ill. She didn’t have a strong support system at home and was often the caretaker for her mother. That stress of being the caretaker made her very much at risk for preterm delivery.”
When it comes to addressing the challenges of psychosocial issues and the stress that pregnant women face, Signature Medical Group has shown that interdisciplinary coordination and integrating care among medical teams has helped.
Signature Medical Group’s implementation of CMS’s Strong Start for Mothers and Newborns initiative focuses on improving health outcomes among mothers and newborns at risk of preterm birth. By focusing on preventing health problems and initiating prenatal care earlier, medical practices can bring in psychosocial and community resources that can boost outcomes and reduce the costs often associated with premature births and neonatal intensive care unit (NICU) services.
In February 2012, CMS first announced the goals of the Strong Start for Mothers and Newborns Initiative, which included both a funding opportunity for healthcare providers as well as a method for generating greater awareness among families about the risk of preterm labor.
The funding opportunity was meant to help pregnant women who are Medicaid recipients or on the Children’s Health Insurance Program (CHIP) reduce their risk of premature births. The results at Signature Medical Group have been positive, said Jim Gera, Senior VP of Business Development at Signature Medical Group.
The results of the maternity care home model
When asked if the Strong Start for Mothers and Newborns initiative reduced the rate of premature births at Signature Medical Group, he answered, “We reduced our preterm birth rate by 20 percent compared to our historical Medicaid preterm birth rate and by 14 percent compared to all births in Missouri. We also are collecting data on maternity HEDIS and quality measures, which are important metrics for payers. We average in the mid to high 80s on HEDIS measures.”
“Overall, no matter what environment we worked in with our care model, whether it’s been a rural, urban or suburban area in every location, we’ve seen a reduction in the overall preterm birth rate,” he continued. “One of the primary reasons we’ve been able to do that is that we’ve deployed a comprehensive biopsychosocial care model in which we’re not only addressing the medical condition like gestational diabetes, but we’re also addressing psychosocial needs such as toxic stress, trauma, and challenging life situations.”
The solutions that reduced the preterm birth rate
Gera detailed the type of solutions the medical practice is using to bring these beneficial outcomes and reduce the rate of premature births. Using this care management model, a provider is able to build more trust with patients and a stronger relationship can ensue. Signature Medical Group uses an interdisciplinary team including the OB/GYN clinical team, licensed social workers, and nurses to help pregnant women address their various medical and psychosocial needs.
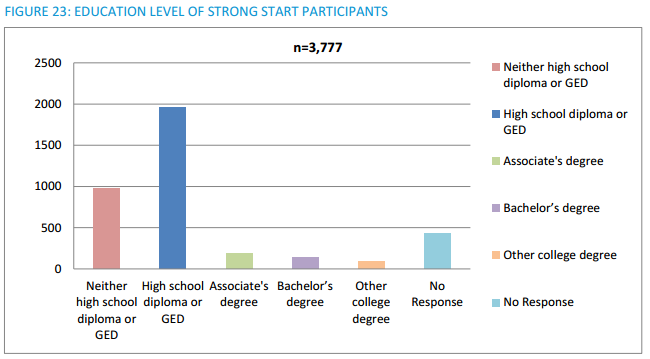
According to the CMS’ first year results of the Strong Start for Mothers and Newborns initiative, the prenatal care models being used have a strong focus on relationship-centered care. Greater emphasis is put on relationships between participating mothers and care providers. The participants were also found to have high levels of psychosocial and emotional needs, which the care models were created to address. Surveys of income and education also suggest that the participants may face larger difficulties in caring for themselves during their pregnancy and post-partum.
Maribeth Hollinshead, the maternity care home model Program Director and Nurse Navigator at Signature Medical Group, also discussed the solutions that the organization used while participating in the CMS initiative to improve outcomes among pregnant women.

“Eligible patients are pregnant Medicaid beneficiaries. We are seeing at-risk and high-risk patients, we do not discriminate against women who are at-risk for a preterm births or have high-risk medical factors including: multiple gestation, preeclampsia, and a history of preterm deliveries,” Hollinshead described. “There’s always been that missing piece and the missing piece is being able to address the psychosocial needs throughout the women’s pregnancies and postpartum period. By addressing those needs, we have the opportunity to change their lives for the better.”
How maternity care costs were reduced
Some other beneficial outcomes of the maternity care home model relate to the fewer newborns in need of NICU services, which was a major area in which costs were reduced. The utilization of NICU was reduced by 24 percent compared to Missouri data, explained Gera. “We have less patients going to NICU because they’ve delivered their babies at full-term or only a week or two early. We’ve also reduced the number of days that patients need to spend in NICU.”
“We were able to engage women earlier in their prenatal care. On average, we initiated prenatal care two weeks earlier than our benchmark when the program began,” he described the program. “The other savings come from more of our patients delivering babies at full term which is considered to be 37 weeks or more. One of our goals to reduce preterm birth costs was to move our patients who would have delivered at 30 or 32 weeks, for example, to 34 or 36 weeks or more. By getting the babies closer to full term preterm birth costs are reduced. As a result, our current average gestational age at birth is just under 39 weeks.”
“We estimate we have saved Missouri $10 to $15 million during the program as a result of implementing our maternity care home model,” he concluded. “Not only are we reducing the cost directly through reduced preterm births and reduced NICU utilization but patients are entering prenatal care earlier, and we are collecting a lot of the metrics necessary for payers in order to demonstrate the value of the program.”
Image Credits: Centers for Medicare & Medicaid Services, Signature Medical Group
Dig Deeper:
How to Overcome the Challenges of Bundled Payment Models
Why Maternity Care Needs Episode-Based Bundled Payments