How Healthcare Payers Could Reduce Wasteful Spending
Payers could decrease wasteful spending through value-based care, software tools, a focus on wellness, and population health management.

- For many years, the health insurance industry has been working to address wasteful spending among hospitals and medical practices. Some of the areas of wasteful spending relate to duplicative medical testing, unnecessary diagnostics, and excessive paperwork.

The American Health Policy Institute released a report describing its work with VBID Health that found unnecessary and wasteful spending account for 20 percent of total funding or about $2 billion among 35 large employers. Prior studies have found that wasteful spending could be responsible for as much as 30 or 40 percent of total healthcare costs.
“This study concludes that over $2 billion of employer healthcare spending is wasteful and unnecessary, out of total spending of approximately $10 billion,” the report stated.
“One objective of this effort is to draw a distinction between high value and low value healthcare services in order to reduce or eliminate wasteful spending. Another goal is to reduce inefficiencies in healthcare delivery and financing, thereby producing greater value. Studies indicate that reductions in wasteful spending resulting in lower costs can also lead to higher quality care.”
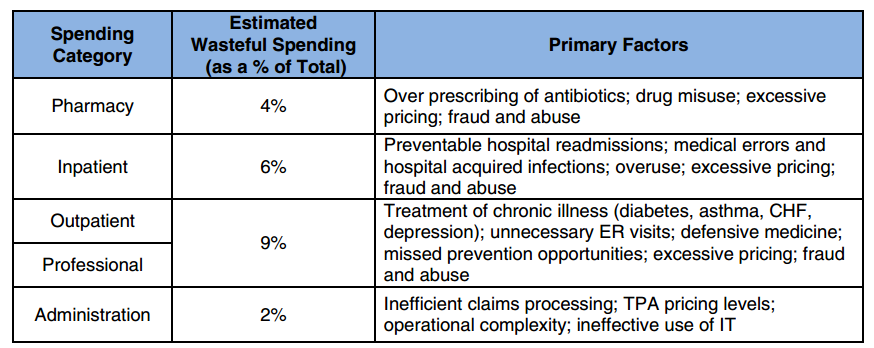
Some of the specific challenges that lead to further wasteful spending revolve around overprescription of drugs and non-adherence for medication regimens. This led to 4 percent of wasteful healthcare spending while hospital-acquired infections, preventable hospital readmissions, and other medical errors brought in 6 percent of unnecessary spend.
The report from the American Health Policy Institute provides some key solutions for addressing wasteful spending within the medical industry. For instance, payers would benefit from using software like the Health Waste Calculator to determine the costs of care at much smaller levels on a per-member per-month basis as well as target spending at specific rates.
Data analysis and quality reporting play a role in reducing wasteful spending. The report advises stakeholders to create score cards with claims data to show the spending areas that have been successful and other services that need improvement.
Another suggestion from the American Health Policy Institute urges payers and provider to move steadily from fee-for-service payment structures toward value-based care reimbursement models.
For example, specific specialties like cardiac treatment, maternity care, or orthopedics have benefited from episode-based bundled payment models. UnitedHealthcare is one payer that has seen a reduction in hospital readmission rates and lengths of stay after implementing bundled payments for orthopedic care.
There are multiple value-based care platforms that payers can take up to reduce unnecessary spending including accountable care organizations, pay-for-performance, and episode-based payments. Michelle Lobe, Vice President of Network Strategy and Innovation at UnitedHealthcare, explained the various value-based care programs that UnitedHealthcare has adopted.
“We have a number of value-based programs all along a continuum starting with the performance-based program where we contract with our hospitals and physician groups and set quality targets for performance,” Lobe said earlier this month. “We have moved into different types of value-based programs. Bundles are becoming much more popular.”
“We also have accountable care organizations. Some are shared risk arrangements and some are shared savings arrangements,” Lobe mentioned.
Payers are also advised to change care plans to emphasize wellness and disease prevention. For instance, payers could send reminders in the mail so that members don’t forget yearly physicals and cancer screening guidelines. Also, payers could educate their consumers to reduce wasteful spending by encouraging the use of primary care and urgent care instead of emergency room visits.
Population health management is another important avenue that payers can use to reduce wasteful spending. For example, through predictive modeling, payers could identify high risk members, rank the costs associated with their care and find solutions to prevent unnecessary treatment or testing for these patients. This may also include improving price transparency throughout their provider network so that a patient who needs an MRI or CT scan can find the most affordable option.
Private payers can also look to the Centers for Medicare & Medicaid Services (CMS) when attempting to cut down on wasteful healthcare spending. Last month, CMS announced a reduction in the Medicare fee-for-service improper payment rate from 12.1 percent to 11 percent over the last year. CMS used provider education and greater oversight to achieve these outcomes.
Commercial payers are advised to use these steps to reduce wasteful spending across the healthcare continuum as well as improve quality and patient outcomes.