How ICD-10 Diagnosis Coding Impacts HEDIS Quality Reporting
Due to the greater intricacy and detail of ICD-10 codes, it is expected to help improve the analysis and measurement of HEDIS quality performance scores.

- On October 1, 2015, healthcare providers and payers across the entire nation switched over to ICD-10 diagnosis coding and left the ICD-9 coding behind. Today the ICD-10 diagnosis coding system is being used for medical claims processing by health payers as well as HEDIS quality measure reporting.
The National Committee for Quality Assurance (NCQA) offered healthcare organizations some tips on their website for developing a system to help identify which ICD-10 codes relate to each HEDIS quality measure.
While other countries moved over to the new ICD-10 diagnosis coding years ago, the US has stuck with ICD-9 codes for much longer, which were first established in the 1970s. It may have been simpler for other nations to switch to the new ICD-10 diagnosis coding system earlier due to the fact that universal healthcare platforms are established in these regions.
In the US, however, healthcare payers also depend on the diagnostic codes used within hospitals and other medical facilities. The NCQA has been helping payers and providers switch over to the new ICD-10 diagnosis coding system since 2011 when they began converting affects HEDIS quality measures to account for the new codes.
In July 2013, NCQA posted to its website the proposed ICD-10 codes affecting quality measures and requested public feedback. Over the years, the organization has phased out the obsolete ICD-9 codes from its HEDIS quality measure reporting requirements.
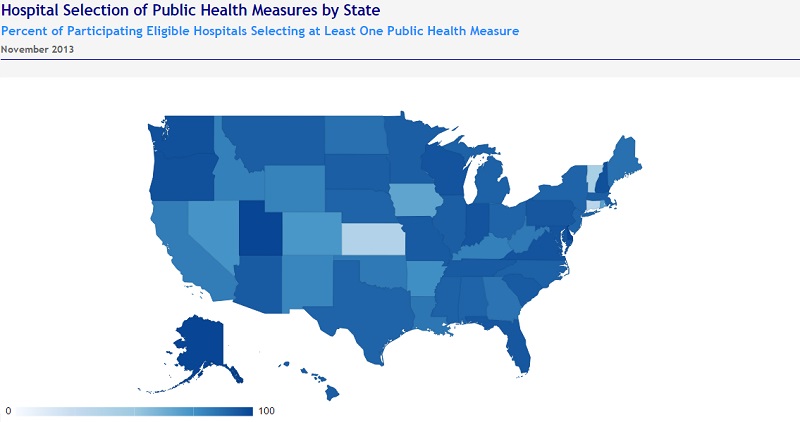
NCQA’s Product Development expert Lori Andersen also offered her opinion on how ICD-10 diagnosis coding will affect HEDIS quality reporting in the coming years. Andersen explains that HEDIS quality measures use medical claims data and the related diagnosis codes to find certain at-risk patients in the population or identify certain health events such as an epidemic. Public health reporting is an important aspects of these measures and the map below shows the percent of hospitals per state reporting on at least one public health measure.
“On October 1, health care providers will begin to use ICD-10 codes to identify diagnoses and procedures on claim forms. HEDIS measures use codes from claims data to identify members in the eligible population or to identify numerator events,” Andersen began. “The increased specificity of ICD-10 codes could significantly improve performance measurement; they can measure concepts that the ICD-9 codes could not.”
An example is a HEDIS quality measure that looks at blood pressure and the served patient population who have hypertension. In particular, the quality measure determines which percentage of the population has controlled blood pressure rates.
Starting on October 1, healthcare providers have been required to use ICD-10 codes on their claims data to track information about outpatient visits related to hypertension. In this way, the HEDIS quality measures related directly to the integration of ICD-10 codes in the healthcare field.
To help providers better understand which codes were being affected by the new ICD-10 diagnosis coding system and how they related to HEDIS quality measures, NCQA published General Equivalence Mappings (GEM) on their website for individuals to find which ICD-10 codes align with the previous ICD-9 version used in HEDIS quality measures.
Also, Andersen mentioned that the NCQA HEDIS Expert Coding Panel verified all of the new ICD-10 codes and published them for public feedback. When determining which ICD-10 codes to apply to the HEDIS quality measures, the organization used best practices offered by the National Quality Forum (NQF).
To download and learn more about the best practices for updating HEDIS quality measures alongside the transition to ICD-10 diagnosis coding, providers and payers should take a look at the NQF website.
When asked whether organizations would be able to continue using ICD-9 codes after the October 1 ICD-10 transition for reporting HEDIS performance measures, Lori Andersen clarified, “Although we expect most organizations to start using ICD-10 codes on October 1 (and do not expect to see ICD-9 codes on claims after that date), HEDIS 2016 specifications do not limit the use of ICD-9 codes (for HEDIS reporting) to before October 1, or limit the use of ICD-10 codes (for HEDIS reporting) to on or after that date.”
“If an organization uses ICD-9 codes after October 1, any ICD-9 codes included in the measure specifications can be used for HEDIS reporting (even with a date of service on or after October 1). However, organizations that are not using ICD-10 codes by the time the ICD-9 codes are removed from measures will not be able to report.”
Due to the greater intricacy and detail of ICD-10 codes, it is expected to help improve the analysis and measurement of HEDIS quality performance scores. “They can measure concepts that the ICD-9 codes could not,” mentioned Andersen.
For instance, when it comes to identifying patients with either severe or mild asthma problems, ICD-10 codes are more specific and provide a greater wealth of information. ICD-9 codes did not offer data on severity and HEDIS quality measures had to rely on the number of doctor visits and prescribed medications to determine which patients were at greatest risk.
However, ICD-10 codes show both “severity (mild, moderate, severe) and duration (intermittent, persistent),” Andersen clarified.
“This has the potential to simplify the method of identifying persistent asthmatics over time,” she continued. “Rather than reviewing visits and medication use over a two-year period, organizations could identify members with persistent asthma through a single visit with an appropriate diagnosis code.”
This shows that ICD-10 codes can be much more useful for assessing general health within a given population and provides more data for assessing HEDIS quality performance scores.
As the healthcare industry from payers and federal agencies to primary care providers and specialists continues to utilize ICD-10 diagnosis codes for claims processing, HEDIS performance reporting will become more precise and push forward a greater focus on quality care.
Image Credit: Office of the National Coordinator for Health IT
