How Medicaid Expansion Improves Behavioral Healthcare Access
At this moment in time, 30 states and the District of Columbia did pursue Medicaid expansion, but 20 states have still not expanded the program.

- When the Patient Protection and Affordable Care Act was passed into law, it established that Medicaid expansion across all 50 states would take place. However, a Supreme Court ruling created a clause that allowed Medicaid expansion to be optional for each state. Many state governors cited cost concerns and went without Medicaid expansion.

This could, however, have a negative impact on low-income individuals unable to cover the costs of health insurance and also ineligible for the Medicaid program. In particular, it could impact patient access to behavioral health services.
Yesterday, the Department of Health and Human Services (HHS) announced in a press release that Medicaid expansion allows states to “greatly improve” behavioral healthcare access. The Affordable Care Act’s provision for Medicaid expansion could be a significant boon to the patient community.
With substance abuse problems and mental health conditions plaguing many neighborhoods around the country, broadening Medicaid coverage across more individuals could be key to solving these important health crises.
“Today’s report shows that Medicaid expansion is an important step states can take to address behavioral health needs, including serious mental illness and opioid and other substance use disorders,” HHS Secretary Sylvia M. Burwell said in a public statement.
The report from HHS outlines that, in 2014, 1.9 million people without health insurance and suffering from a mental health illness or substance abuse issue lived in states that did not expand Medicaid coverage as proposed by the Affordable Care Act. All of these individuals would also be eligible for the Medicaid program if it was broadened under Obamacare’s provisions in each state.
Out of all low-income uninsured people in these states that haven’t expanded Medicaid, almost 30 percent are in need of behavioral health services, according to the report. Some of these low-income individuals did have access to health insurance in 2014, but a large number will gain coverage only if Medicaid expansion takes place in their states while others would be able to purchase “more affordable coverage,” the HHS press release states.
At this moment in time, 30 states and the District of Columbia did pursue Medicaid expansion, but 20 states have still not expanded the program to provide healthcare coverage for those with a low income. However, these 20 states would benefit greatly from Medicaid expansion, HHS explains in the release.
Research shows that more than 4 million Americans will lack healthcare coverage in 2016 if these states continue to deny Medicaid expansion. Among its many benefits, expanding the Medicaid program, as stated in the report, will lead to treatment access among those suffering from substance abuse and mental health conditions.
If the healthcare industry is looking to improve health outcomes and assist those lacking necessary treatment, it’s vital to increase insurance coverage and expand the Medicaid program in 20 states that have declined to participate in this particular clause of the Affordable Care Act.
The HHS report explains that 371,000 less people would suffer from depression annually if all states broadened their Medicaid coverage and 540,000 more would “report being in good or excellent health.”
“Medicaid expansion provides the opportunity to address the complicated physical and behavioral health needs of those it covers. Behavioral health conditions are costly to treat and are also associated with other medical costs,” the HHS report stated.
“More than 68% of adults with mental illness are reported to have at least one general medical disorder, which is a substantially higher rate than for individuals without mental illness. Improved access to care would improve the health and well-being of this population and in some cases produce savings. For example, for individuals with depression and diabetes, researchers found that improved treatment of depression not only led treated individuals to fewer days with depression, but also resulted in lower overall outpatient medical costs.”
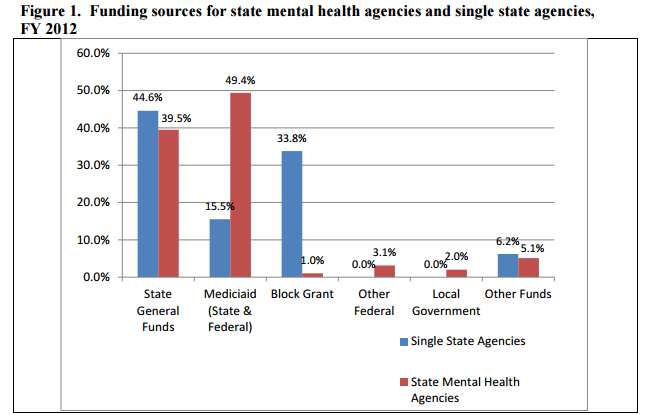
Additionally, HHS advises that behavioral health programs would likely improve without risking new costs if Medicaid expansion is incorporated. More funding would be funneled into state mental health agencies.
States that expand their Medicaid programs can also benefit from a “more productive workforce,” HHS mentions, as better mental healthcare and substance abuse treatment should keep employees less likely to miss work.
Even those suffering from depression have taken more disability days off from work than those who aren’t debilitated by the condition, research shows. As such, increasing Medicaid coverage and boosting behavioral healthcare access could help employers keep a stronger workforce.
“Research studies have found reductions in the number of workers with substance use disorders who missed work, were late for work, were less productive than usual or had a conflict with management or a coworker after employees accessed specialized treatment,” the report said. “Substance use disorder treatment was associated with $5,366 annually in employer savings from reduced absenteeism alone.”
Essentially, expanding the Medicaid program across the rest of the states could be a major boost to behavioral healthcare access, which could positively affect both businesses and families.
Image Credits: Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation