MA Proposed Rule May Cut Savings from Ambulatory Surgery Centers
Research suggests that health payers can garner more savings by utilizing ambulatory surgery centers for outpatient surgery instead of hospital departments.

- New proposed changes to current legislation from the Massachusetts Department of Public Health may either decrease the use of or potentially eliminate ambulatory surgery centers, according to a press release from Healthcare Bluebook. The reason health payers need to be aware of this occurrence is because ambulatory surgery centers significantly reduce the cost of outpatient surgery and the proposed changes could impact healthcare spending and access to care.

In fact, Healthcare Bluebook released a study of private health insurance claims showing that ambulatory surgery centers cut the cost of outpatient surgery nationwide by more than $38 billion annually. The study also outlined that Medicare costs were reduced by more than $7 billion when services were rendered at ambulatory surgery centers between the years 2007 to 2011. Essentially, ambulatory surgery centers offer a lower cost of care when compared to hospitals and their outpatient departments.
Payers in the state of Massachusetts share $793 million of those cost savings based on population size, which means that the Massachusetts Department of Public Health’s proposed rulings could decrease those savings by eliminating the reliance on ambulatory surgery centers.
Not only would payers have to manage the spending associated with this policy change, but patients and employers in Massachusetts may also see higher prices, the press release states.
“Requiring ASC’s to partner with hospitals before building new facilities is like requiring Boston Burger Company to partner with McDonald’s before opening new restaurants,” Bill Kampine, Senior Vice President for Healthcare Bluebook, said in a public statement.
“Competition keeps healthcare costs low and independent ASC’s are a cost-effective alternative to hospital outpatient departments. In Boston, for example, the total price for a knee arthroscopy can be $8,500 or more at a hospital outpatient department while the price for the same procedure at an ASC can be as low as $3,500. Without ASC’s, patients and employers that sponsor their health plans can expect to pay more for outpatient procedures,” concluded Kampine.
The study found that the cost of the same services at ambulatory surgery centers were significantly lower than the prices of the services at hospital outpatient departments across all insurers. The study used commercial claims data from 2014 for analysis of more than 400,000 policyholders countrywide. When analyzing the data, the researchers did adjust for high-risk patients who were not eligible for outpatient surgery in ambulatory surgery centers.
The study shows that health payers pass down the savings from ambulatory surgery centers down to the consumer. As much as $5 billion of savings are passed to the consumer through lower deductibles and coinsurance payments.
Additionally, the report finds that ambulatory surgery centers could save an additional $17 billion if these outpatient facilities were utilized in most cases a patient may be eligible for. For example, insurers may see more cost savings if procedures like total joint replacement surgeries are conducted at ambulatory surgery centers.
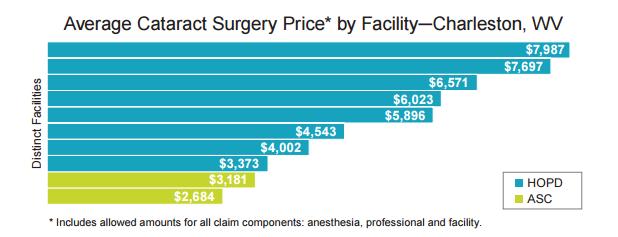
The study even outlined how prices for cataract surgery in the same cities could vary threefold. This shows that healthcare payers may need to bring more attention to price transparency and encourage their consumers to pursue medical care in affordable, high-quality medical facilities.
This past summer, a report from the Ambulatory Surgery Center Association also found that these facilities tend to have lower reimbursement rates than outpatient hospital departments. The research suggests that public and private payers reimburse ambulatory surgery centers less than hospital outpatient departments for the same services.
The potential reason for the lower reimbursement rates is due to the fact that hospital outpatient departments are connected to multiple departments and healthcare providers, which offers them more leverage in negotiating their contract rates.
“As premiums rise and adoption of high-deductible health plans increases, patients have greater incentives to reduce their costs by choosing ASC-based care, but education is lacking,” the study from the Ambulatory Surgery Center Association stated. “Though healthcare transparency has made significant advancements in recent years, most patients are still unaware of the lower costs that ASCs offer.”
Ambulatory surgery centers looking to ensure a stronger revenue cycle may need to include data analytics in their EHR functionalities, said Dr. Scott Ketover, the President and Chairman of the Board of Digestive Health Physicians Association (DHPA) as well as the President and CEO of Minnesota Gastroenterology.
“Within our practice we have an EHR that we’ve been using for a long time across our offices. The system has been helpful to our providers in knowing patient history and providing quality care. EHRs themselves definitely go a long way in improving patient care,” Ketover told EHRIntelligence.com.
Additionally, medical billing staff will need full training in all new revenue cycle systems implemented in order to reduce the likelihood of claim denials.
Healthcare payers looking for more affordable outpatient surgeries for their consumer base may need to begin encouraging the use of ambulatory surgery centers among their policyholders.
Image Credits: Healthcare Bluebook
Dig Deeper:
Ambulatory Surgery Centers Decrease Costs by $38 Billion
Time, Commitment Required for ACO, Value-Based Care Success