MACRA Pushes Payers to Adopt Value-Based Care Payment Models
With providers focused on meeting MACRA regulations, commercial payers are investing in value-based care payment models that align with the quality payment program.

- This past summer, the Labor Department announced that healthcare spending rose in August more steeply than at any point in more than 30 years. The costs for medical treatment grew by 1 percent in just one month, the Los Angeles Times reported. With such significant increases in healthcare costs, payers and providers may need to work further in advancing value-based care payment models.

Value-based care payment models are likely to become more and more common among payers and providers due to MACRA regulations and the focus on alternative payment models from the Centers for Medicare & Medicaid Services (CMS). Payers would benefit from partnering with providers that are serious about improving quality of care and engaging in value-based care payment instead of staying with fee-for-service strategies.
Today providers are looking to partner with payers in value-based care payment models like bundled payments or shared savings through accountable care organizations (ACOs).
“We have a very large accountable care organization participation and many of those that are participating with private payers in ACO-like arrangements had hoped for more opportunities. There are opportunities with payers already but we do believe that opportunities would pick up the pace,” Danielle Lloyd, MPH, Vice President of Policy & Advocacy and the Deputy Director DC Office at Premier Inc., told HealthPayerIntelligence.com.
“The main issue is to make more models available to providers since many are eager to enter these type of programs and are looking for partnerships with payers,” Lloyd concluded.
With providers taking up MACRA implementation and embracing the quality payment program, CMS Acting Administrator Andy Slavitt explained at the MACRA MIPS/APM Summit earlier this month that the healthcare industry is continually moving toward value-based care payment.
Some of the ways that CMS is supporting value-based care reimbursement includes a focus on patient-centered care, advancement of health IT interoperability, and the ongoing work at the CMS Innovation Center, said Slavitt.
In case of an Affordable Care Act repeal, the CMS Acting Administrator urged commercial payers to continue on the progress of value-based care by offering preventive care without out-of-pocket costs, keeping patients with pre-existing conditions covered, and eliminating lifetime limits.
One of the key ways that the federal government was able to advance value-based care payment models was through the CMS Innovation Center, emphasized Slavitt. For cost reduction, the Innovation Center and its value-based care payment models are key. The Congressional Budget predicts that the center and its programs will cut federal spending by $34 billion over the following 10 years.
“I’ll say this bluntly: MACRA can’t work as well without a CMS Innovation Center that can move quickly to develop and expand new approaches to paying for care,” Slavitt said at the MACRA MIPS/APM Summit. “With changes to the Innovation Center, the advanced alternative payment approaches could slow significantly. We will have a much narrower path with fewer specialty options and approaches, which take in patient and physician feedback. Medicare and commercial payers would then fall further out of alignment, and more importantly, less patients would have access to innovative care methods.”
Commercial payers have been following the CMS lead and investing in value-based care such as bundles and shared savings in recent years as well. For best results, payers may need to partner with hospital systems aimed at reducing spending and implementing value-based care payment models.
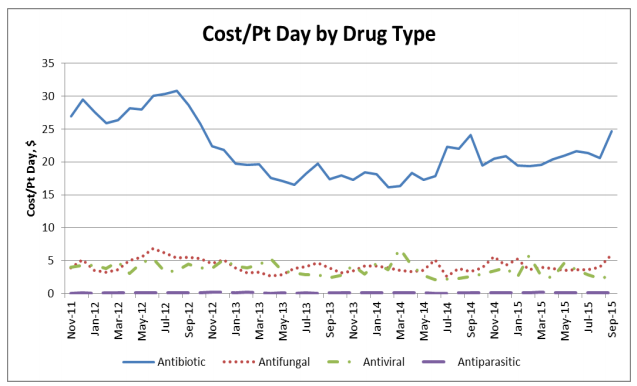
The Ohio State University Wexner Medical Center is one example of a provider looking to improve the quality of care in an effort to cut down on wasteful spending. The Ohio State medical center has used clinical data to analyze the intake of antimicrobial medication, according to the Healthcare Information and Management Systems Society (HIMSS).
The work at this medical center led to a reduction in C. difficile infection rates. The healthcare system was able to significantly decrease antimicrobial costs per patient days from September 2012 to September 2015. Additionally, health maintenance alerts helped clinicians at the Ohio State University Wexner Medical Center boost chronic disease management and raise the number of diabetic patients with HgbA1c under control by 5 percent.
The HealthNet of Indianapolis also reached key healthcare quality targets in 2014, HIMSS stated. For example, asthma pharmacologic therapy was reached for 89 percent of the federal clinical quality measures while weight assessment was reached for 73 percent and adult tobacco cessation counseling measures reached 100 percent.
With more providers focusing on the quality payment program and meeting MACRA regulations, payers will need to move forward with contracting through value-based care payment models.
Image Credits: HIMSS
Dig Deeper:
How Payers Should Prepare for Value-Based Reimbursement
Key Steps for Payer Success in Accountable Care Organizations