Managed Care Accounted for 38% of Medicaid Spending in 2012
Medicaid managed care spending accounted for 38 percent of program expenses in 2012, representing an increase in program spending per beneficiary.

Source: Thinkstock
- Medicaid managed care accounted for 38 percent of total Medicaid spending in 2012, according to a Congressional Budget Office analysis.
The report found that the majority of states in the US have implemented some form of a managed care program for their Medicaid beneficiaries.
In 2014, thirty-three states established statewide general comprehensive managed care programs under the ACA’s Medicaid expansion. Only three states including Alaska, Connecticut, and Montana implemented Medicaid expansion with a fee-for-service system.
From 1999 to 2014, the number of states that spent over 25 percent on managed care grew from five to thirty states. CBO said that this number grew as more states opted to expand Medicaid under the ACA. Additionally, the number of states that spent 50 percent or more on Medicaid managed care increased from two to thirteen states.
The analysis suggests that states may not be using managed care to effectively address Medicaid spending challenges and improve the outcomes of enrollees.
Ninety-one percent of non-elderly, non-disabled adult Medicaid beneficiaries were enrolled in an MCO in 2012. MCOs spent $46.7 billion on healthcare services for these adults, while fee-for-service spent an additional $7.3 billion to help cover services.
Source: Congressional Budget Office
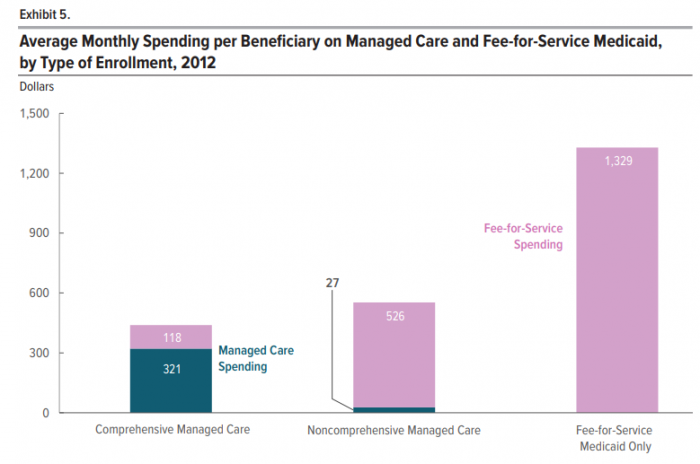
In 2013, 73 percent of average monthly spending on Medicaid comprehensive managed care was for MCO-administered care. Only 5 percent of average monthly spending for non-comprehensive managed care went to MCOs because non-comprehensive MCOs only cover limited enrollee benefits.
“The fact that such an overwhelming share of spending for Medicaid beneficiaries enrolled in non-comprehensive managed care—who accounted for more than one-quarter of all Medicaid beneficiaries—goes to fee-for-service Medicaid helps to explain why spending for managed care is so much less than spending for fee-for-service Medicaid despite the high rate of enrollment in managed care,” CBO said.
The report also found that fee-for-service covers a greater portion of care costs for older and more vulnerable beneficiaries.
Managed care only pays 36 percent of care costs for elderly and disabled beneficiaries in Medicaid, and only 16 percent of costs for dual-eligible Medicaid-Medicare beneficiaries. Older beneficiaries are a minority within the Medicaid program but contribute to the program’s highest healthcare costs.
In 2012, the average monthly cost for elderly and disabled Medicaid beneficiary services was $1,602. Average spending was $1,402 per month for Medicare-Medicaid dual-eligible beneficiaries.
Medicaid managed care covers the majority of costs for non-elderly, non-disabled adults and children, leaving fee-for-service to cover more expensive beneficiary groups.
“Although 77 percent of Medicaid beneficiaries in 2012 were nonelderly, nondisabled adults or children, they accounted for only 35 percent of Medicaid spending; beneficiaries who were enrolled in Medicare and other elderly and disabled beneficiaries constituted 23 percent of Medicaid beneficiaries but accounted for 65 percent of spending,” CBO explained.
States may want to re-evaluate how their managed care contracts are structured, since managed care rarely addresses Medicaid’s most expensive beneficiary populations. Managed care has increased in scale over the last decade, but has done little to reduce spending within Medicaid’s high-risk populations.
“States might implement Medicaid managed care for a variety of reasons,” CBO said. “Two of the most often cited are to increase the predictability of spending and to improve the coordination of care. Proponents of managed care suggest that competition between MCOs reduces spending and improves outcomes. To date, however, studies of managed care have not found consistent evidence to support those claims.”
