Medicaid Challenges with Value-Based Care Payment Models
The report elucidates how the Medicaid Program is moving toward value-based care payment models and leaving fee-for-service reimbursement in the dust.

- With the federal government and the healthcare industry as a whole focusing their efforts on adopting value-based care payment models that revolutionize medical care, it should come as no surprise that the National Association of Medicaid Directors (NAMD) released a report outlining how to connect healthcare payment to clinical care delivery.

The Bailit Health Purchasing and The Commonwealth Fund contributed to the report, which discusses vital state Medicaid strategies that could connect the quality of care to reimbursement, according to a press release from NAMD.
The report is called The Role of State Medicaid Programs in Improving the Value of the Health Care System and it elucidates how the Medicaid Program is moving toward value-based care payment models and leaving fee-for-service reimbursement in the dust.
“Value-based purchasing is quickly becoming the new paradigm in Medicaid,” Tom Betlach, NAMD’s President and Director of the Arizona’s Medicaid program, stated in the press release. “States recognize that we must sever the link that has historically tied reimbursement to the quantity of services delivered, not the outcomes we want for Medicaid consumers. This will be a multi-year progression as states and providers evaluate and refine these models.”
The report looked at 34 states to make its analysis. Approximately 67 percent of the state Medicaid programs analyzed are working on creating new reimbursement protocols at the provider level. NAMD has expressed its viewpoints to the Department of Health and Human Services (HHS) secretary Sylvia M. Burwell by urging the alignment and acceleration of innovations related to State Medicaid work alongside federal agencies.
“As our report shows, Medicaid Directors strongly support HHS’s efforts to move to a healthcare system that rewards quality and improved health outcomes,” NAMD’s Executive Director Matt Salo mentioned in the release. “Medicaid programs are a critical component of those efforts, and bring a breadth and depth of experiences to the national conversation on delivery system reform. Directors across the country, while moving forward with innovation in their states, look forward to further collaboration between HHS and state Medicaid agencies.”
It is also important to note that this report outlines the obstacles that state Medicaid programs are forced to manage when switching provider reimbursement to value-based care payment models. For example, there is technically a policy conflict between the reimbursement of safety net clinics and the quality benchmarks of value-based care payment models.
Medicaid Directors are also focused on reinvesting savings in healthcare quality improvement. In the cover letter to the report, NAMD Discussed how growing healthcare costs and a rise in patient populations are causing more pressure for Medicaid and Medicare programs. This has led to a greater need for adoption of value-based care payment models and alternative reimbursement in order to better manage these issues.
Whether through managed care or contracting directly with healthcare providers, state Medicaid programs are attempting to move reimbursement away from fee-for-service payment systems toward rewarding value.
There are specific areas in which these Medicaid alternative Payment Systems fall into. These include episode-based care or bundled payments, population-based payments, And other reimbursement forms that assist in delivery system reform. The National Association of Medicaid Directors urges Centers for Medicare and Medicaid services CMS to move toward aligning in its differing programs and models through the Centers for Medicare and Medicaid Innovation.
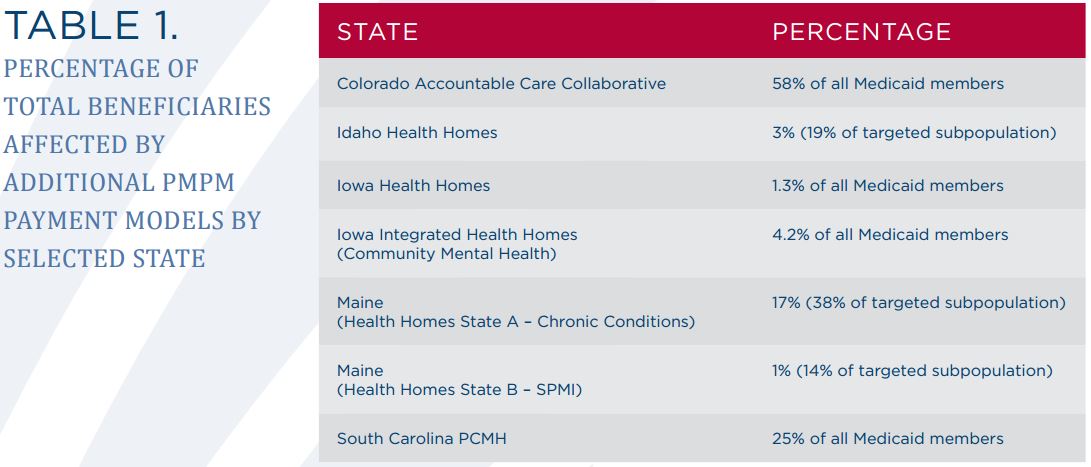
The report outlines that state Medicaid leaders should address the fact that moving toward value-based care payment models is often a very difficult and complex process. Most importantly, state Medicaid leaders should focus on ensuring the health outcomes of their beneficiaries is improved. The NAMD also looked at how many beneficiaries have been impacted by per-member, per-month payment models.
Additionally, Medicaid directors should be aware that high-quality data is a necessity in a value-based care environment.In general, alternative payments rely on high-quality data, as healthcare quality improvement efforts and care coordination rely on sharing essential, timely data.
When designing alternative payment models, Medicaid leaders are encouraged to bring in stakeholders in the early part of the process. In addition to keeping stakeholders aligned with Medicaid innovations, it is vital to ensure that multi-payer reform takes place, as federal programs that aren’t coordinating with Medicaid efforts could potentially hinder the effectiveness of payment transformation on a state level.
Along with multi-payer reform initiatives, new rate setting changes may need to be incorporated in the managed care setting when integrating alternative payment systems. The report also found that a majority of state Medicaid efforts to move toward value-based payment is centered around primary and acute care facilities.
“A number of states are using wider-scale alternative payment models as a way to further change the incentives from volume to value. Efforts range from statewide mandated payment changes to experimental pilot programs,” the report from NAMD stated.
“States are implementing these models in three different ways. First, some states are designing their own alternative payment models and contracting directly with providers through the traditional Medicaid FFS delivery models or through their Primary Care Case Management (PCCM) programs.”
“Second, some states are requiring their MCOs to implement MCO-designed alternative payment models, and, in some cases, are providing MCOs guidance on what the model should include. Lastly, other states are designing their own models and encouraging, requiring or incentivizing their MCOs to implement the state-designed alternative payment model. Today, states are choosing the implementation path and model that makes the most sense for their program, state environment and culture. Regardless of which approach or which model is used, significant work and resources are required on the part of the state, their plans and their providers to realize success.”
State Medicaid Directors looking to effectively incorporate value-based care payment models and succeed in alternative reimbursement may need to peruse this report to further understand the efforts necessary to thrive in the constantly changing healthcare payment landscape.
Image Credits: National Association of Medicaid Directors