Medicare-Medicaid Financial Alignment Shows Cost Savings
Essentially, the Medicare-Medicaid Financial Alignment Initiative is meant to promote a better care experience for dual-eligible members.

- One program led by the Centers for Medicare & Medicaid Services (CMS) called the Medicare-Medicaid Financial Alignment Initiative moves toward improving the coordination and quality of healthcare services within Medicaid health homes while also decreasing the spending related to dual-eligible Medicare-Medicaid beneficiaries known to be “high-risk, high-cost” enrollees. Last week, CMS released a report showing results from the Washington Health Homes demonstration, which was part of the Medicare-Medicaid Financial Alignment Initiative.

With more than 10 million people around the country enrolled in both the Medicaid and Medicare programs, it is vital for CMS to strive toward reducing the costs of care associated with dual-eligible beneficiaries. The Medicare-Medicaid Financial Alignment Initiative will move toward making this happen.
Some of the factors that have made it difficult to improve quality and stabilize cost for dual-eligible beneficiaries “a lack of alignment and cohesiveness between” the Medicare and Medicaid programs as well as “misaligned incentives for payers and providers,” CMS reported. The demonstration from Washington is testing out new methods for improving coordination of services between the Medicare and Medicaid program among Medicare-Medicaid enrollees in the state of Washington.
Washington Health Homes demonstration
The Washington Health Homes demonstration also allows both the state and federal governments to take part in sharing in the savings that accumulate from the quality improvement initiatives.
“The Washington Health Home MFFS demonstration leverages Medicaid health homes, established under Section 2703 of the Affordable Care Act, to integrate care for high-cost, high-risk, full-benefit Medicare-Medicaid beneficiaries. It is jointly administered at the State level by the Washington Health Care Authority (HCA),” the report explained.
“Washington has targeted the Washington Health Homes MFFS demonstration to high-cost, high-risk Medicare-Medicaid enrollees based on the principle that focusing intensive care coordination on those with the greatest need provides the greatest potential for improved health outcomes and cost savings. It is organized around the principles of patient activation and engagement, and support for enrollees to take steps to improve their own health.”
The preliminary results from the Washington Health Homes demonstration span a timeline from July 2013 to December 2014. Even though there hasn’t been a significant amount of time for the study to take place, it still managed to show a large cost savings of $21.6 million for the Medicare program when compared to a control group, which shows at least 6 percent in cost savings.
Once Medicaid healthcare spending results are in, they will be further analyzed and compared to the Medicare cost savings within the health homes demonstration. The report from CMS about the Medicare-Medicaid Financial Alignment Initiative within the Washington partnership also provides an overall discussion about the “initial implementation experience” and “beneficiary focus group findings” as well as population health factors.
The report essentially shows favorable results in the state of Washington with regard to impacting the quality of care along with Medicare spending among “high-risk, high-cost” dual eligible beneficiaries.
Further research findings will show more information from the Washington Health Homes demonstration with greater focus on measuring quality, cost, healthcare access and utilization.
“As a shared savings initiative (i.e., one in which the State may be eligible to share in savings that accrue to Medicare as a result of the demonstration), CMS has worked with the State to align Washington beneficiaries with the demonstration, ensuring that beneficiaries are attributed to only one Medicare shared savings initiative,” the report stated.
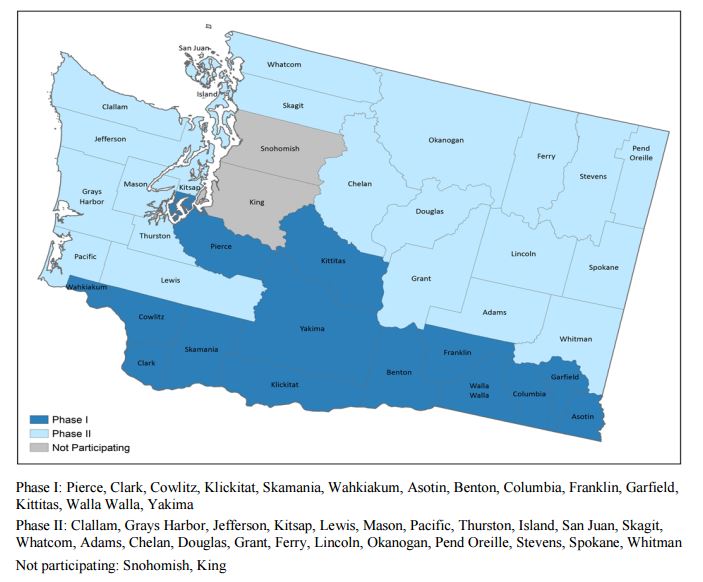
“The State auto-enrolls eligible Medicare-Medicaid beneficiaries who have been attributed to the demonstration into health homes at a rate that can be supported by their care coordination capacity, using zip codes to achieve geographic balance in enrollments.”
Two New Models
Essentially, the Medicare-Medicaid Financial Alignment Initiative is meant to promote a better care experience for dual-eligible members. Throughout the program, CMS will be working with states to implement two models and determine how well the models meet the goals of reducing wasteful spending and strengthening quality of care among Medicare-Medicaid recipients.
The two new models are the Capitated Model and the Managed Fee-for-Service Model. In the Capitated Model, a health plan along with CMS and the state government enters into a three-party contract in which the health insurer will obtain a “prospective blended payment” when it reaches well-coordinated, comprehensive care protocols.
Within the Managed Fee-for-Service Model, the state government and CMS make an arrangement in which the state would potentially share in cost savings that are specifically tied to outcomes from quality improvement and cost-cutting initiatives among the Medicare and Medicaid programs.
“CMS is testing two demonstration models, capitated and managed fee-for-service (MFFS), to better align the financing of these two programs and integrate services for their Medicare-Medicaid enrollees,” the report stated. “Under MFFS model demonstrations such as the Washington Health Home Program, a State and CMS enter into an agreement by which the State would be eligible to benefit from Medicare savings resulting from initiatives designed to improve quality and reduce costs within fee-for-service Medicare and Medicaid.”
The states participating in the Medicare-Medicaid Financial Alignment Initiative include California, Colorado, Illinois, Massachusetts, Michigan, Minnesota, New York, Ohio, South Carolina, Texas, Virginia, and Washington.
The CMS Innovation Center and the CMS Medicare-Medicaid Coordination Office are working together to accomplish the goals of the Medicare-Medicaid Financial Alignment Initiative such as greater coordination in benefits and services among dual-eligible beneficiaries.
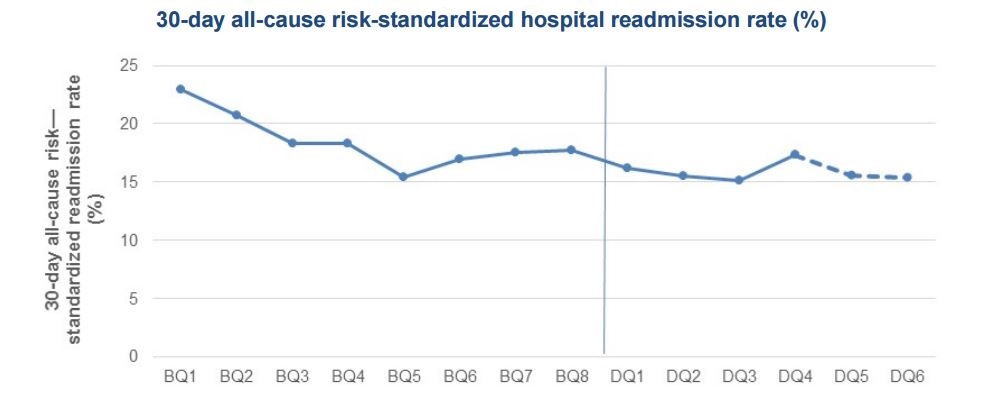
The report from the state of Washington also showed that hospital readmission rates decreased since implementation of the initiative. The cost savings found in the Medicare program due to the Medicare-Medicaid Financial Alignment Initiative in Washington clearly show how these developments have led to more cost-effective and high quality care among the dual-eligible beneficiary population.
Image Credit: RTI International