New Framework for MACRA’s Alternative Payment Models Released
The MACRA legislation expects the Merit-Based Incentive Payment System to cover reimbursement in a multi-payer fashion including both Medicare quality reporting and measure systems from private payers.

- Earlier this year, the federal government passed the Medicare Access & CHIP Reauthorization Act of 2015 (MACRA), which reforms the Medicare program by abolishing the Sustainable Growth Rate (SGR) formula, developing a more effective value-based care platform, and consolidating quality reporting programs into one cohesive system.

The Centers for Medicare & Medicaid Services (CMS) report that there are two methods that the MACRA legislation will develop for providers to report healthcare quality metrics. These two methods are the Merit-Based Incentive Payment System (MIPS) and the Alternative Payment Models (APMs).
The Merit-Based Incentive Payment System consists of bringing together multiple quality reporting programs such as the Physician Quality Reporting System (PQRS), the Value Modifier and the Medicare Electronic Health Record (EHR) incentive program all into one single system. Alternative Payment Models consist of new reimbursement methods such as lump-sum incentive payments or bundled payment platforms.
Late last week, CMS released a report called CMS Quality Measure Development Plan: Supporting the Transition to the Merit-based Incentive Payment System (MIPS) and Alternative Payment Models (APMs), which discussed the importance of linking Medicare reimbursement to value-based care payments.
CMS plans to have 30 percent of Medicare claims to be in the form of value-based payments by December of 2016 and 50 percent of Medicare claims in alternative payment models by the end of 2018. The report presented is essentially a framework for meeting these goals and developing a clear path toward creating the Merit-Based Incentive Payment System and the Alternative Payment Models.
Every eligible provider taking part in the Merit-Based Incentive Payment System will receive a payment adjustment in 2019 based on their quality performance scores, clinical practice improvement initiatives, resource use, and meaningful use of EHR technology.
When it comes to clinical practice improvement, in particular, there are several categories the MIPS will be looking at with regard to provider performance. These categories include greater medical practice access, care coordination efforts, population health management, insurance beneficiary engagement, participation in an alternative payment model, and patient safety.
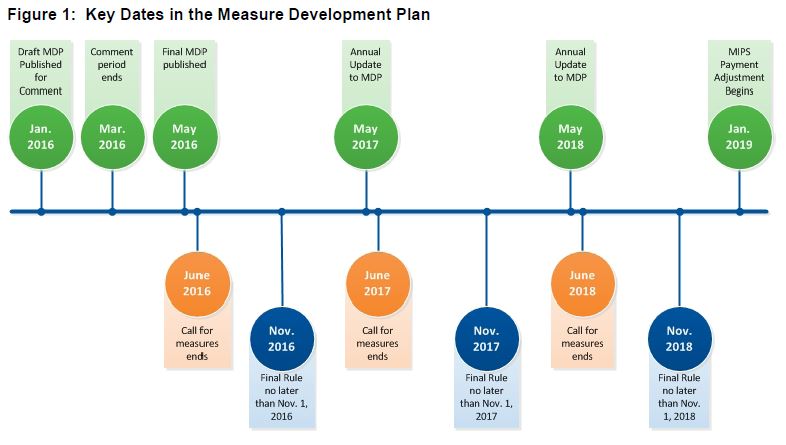
The report details important dates for measure development, which should have a final rule published by November 2018 at the latest after several annual updates. The MACRA legislation expects the Merit-Based Incentive Payment System to cover reimbursement in a multi-payer fashion. This includes both Medicare quality reporting and measure systems used by private payers.
There are five quality domains that providers will need to consider to take part in either the MIPS program or Alternative Payment Models. These domains are:
1) Patient safety
2) Clinical care quality
3) Care coordination
4) Population health management and disease prevention
5) Patient and family engagement and experience
“MACRA further establishes priorities for the types of measures to be developed, which shall include outcome, patient experience, care coordination, and measures of appropriate use of services, such as measures of overuse,” the CMS report mentioned.
The MACRA legislation is focused on a few simple goals of improving quality of care, clinical efficiency, and a general decrease in spending. Additionally, CMS is looking to conduct a gap analysis of any quality performance measures as well as gaps in quality domains across healthcare specialties.
With regard to electronic specifications, the MACRA legislation seeks to incorporate “certified EHR technologies and QCDRs for reporting quality measures,” according to the report.
There are specific obstacles that must also be addressed when pursuing quality measure development plans and these include incorporating patient feedback and engaging patients in measure development, decreasing provider burden, decreasing timeframes for measure formulation, creating meaningful outcome measures, and developing shared accountability measures.
“These policy changes and announcements follow widespread calls to move from the current volume-based fee-for-service (FFS) payment system to a value-based system that pays for patient outcomes rather than individual services,” reported the Physicians for a National Health Program publication.
“Value-based health care should be the goal of any health reform initiative. However, even with SGR out of the way, there are major challenges to achieving that goal, including the lack of an agreed-upon, patient-centered definition of value; a shortage of meaningful performance metrics; and a deficiency of accounting systems capable of reflecting the true cost of delivering care.”
Stakeholders will need to work with the patient community and the payer industry to develop measures that are meaningful and worthwhile for the industry as a whole. Greater alignment between private enterprises, public agencies, the federal government, and the healthcare field is key when creating these measures.
“MACRA requires consideration of how to incorporate measures used by private payers and integrated delivery systems within Medicare quality reporting programs,” the report stated. “The creation and use of measures applicable across payers can lessen provider burden and contribute to improved health outcomes by reducing data capture and measure variation.”
Following the framework set forth in this report to create quality measures and develop a way to reach Alternative Payment Models and the Merit-Based Incentive Payment System will lead to value-based care, greater care coordination, more stabilized healthcare spending, and better quality services across the medical profession.