OH Medicaid Adopts Pass-Through Model for Managed Care Drugs
Ohio’s Medicaid program is transitioning its managed care drug purchasing to a pass-through model, and is asking managed care plans to re-negotiate PBM contracts.

Source: Thinkstock
- Ohio’s Medicaid program has issued a mandate that requires managed care health plans to re-negotiate pharmacy benefit manager (PBM) contracts to transition from a spread-pricing drug purchasing model to a pass-through model.
The state’s five managed care payers are required to implement a pass-through model for drug pricing by the start of 2019.
Currently, Ohio’s managed care plans use spread-pricing models. A spread-pricing model is when a payer purchases drugs based on the difference between the retail price and the PBM’s negotiated rate.
The pass-through structure requires a PBM to charge a managed care plan the exact amount the PBM pays for prescriptions and dispensing fees.
Ohio’s decision to alter how managed care plans purchase pharmaceuticals comes after the state commissioned a consulting company called HealthPlan Data Solutions (HDS) to audit Ohio’s managed care PBMs.
The findings of the June 2018 audit encouraged Medicaid administrators to re-adjust drug purchasing to a pass-through model.
Source: HealthPlan Data Solutions
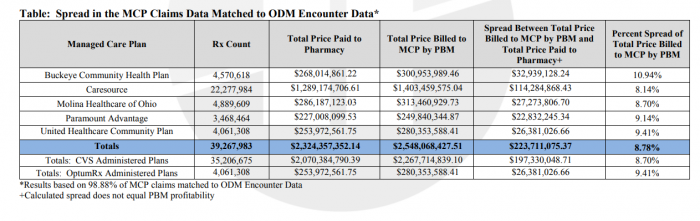
The audit found that in 2017, Ohio PBMs billed managed care payers $223 million more than what the PBMs paid in pharmacy costs. As the largest PBM in the state, CVS Health charged managed care plans $193 million of the total spread.
The transition can save Ohio’s managed care payers nearly $16 million in annual prescription drug costs, according to the audit.
HDS determined that a pass-through model is more likely to generate cost savings for managed care payers, even though pass-through models add an administrative fee of $0.95 to $1.90 for each prescription transaction. The model is expected to generate savings due to guaranteed drug rebates and increased contract transparency.
Ohio’s managed care payers are now working with the state’s Medicaid administration to complete final steps before the pass-through mandate is finalized.
The remaining action items include designing and setting pass-through rates by November 2018 and conducting actuarial analyses to create a budget-neutral program.
Ohio’s Medicaid program assured stakeholders that it will be able to incorporate pass-through purchasing for managed care plans in a timely fashion.
“Ohio Medicaid looks forward to continuing or work to serve Ohioans,” Medicaid Director Barbara R. Sears said. “While I understand this is a large undertaking in a short period of time, I am confident that Ohio’s managed care plans will meet these challenges and implement these changes efficiently and successfully.”
CVS Health, the state’s largest PBM, issued a press statement saying that it is actively working with managed care plans to move to a pass-through model as a beneficial partner.
“PBMs have saved Ohio taxpayers $145 million annually through the services they provide to the state's Medicaid managed care plans,” CVS Health said. “CVS Health will continue to help its Ohio Medicaid clients manage their drug costs and improve their members' health outcomes in 2019 and beyond.”
The annual growth of prescription drug costs nationwide sparked efforts from public payers to find the best solutions to lower drug costs. Medicare is looking to lower drug prices and increase price transparency, while other state Medicaid programs implemented value-based purchasing models for prescription drugs.
