OIG: CMS Overpaid Colorado Medicaid Program More than $38M
Under the CHIPRA legislation, Colorado overstated its enrollment numbers in their Medicaid program and received $38 million in ineligible bonus payments.

- The Office of the Inspector General discovered in an audit that the state of Colorado received millions of dollars in unallowable payments from operating the Medicaid Program and the Children's Health Insurance Program. The report from the Office of the Inspector General states that the Children’s Health Insurance Program Reauthorization Act of 2009 (CHIPRA) enabled more than $3 billion to be given to qualifying states in the form of performance bonus payments between 2009 and 2013.

This was meant to reduce the costs associated with a rising number of children becoming enrolled in the Children's Health Insurance Program. When it comes to CHIPRA bonus payments, the Office of the Inspector General has previously found that it is a high-risk area for unallowable payments.
CHIPRA legislation affects both enrollment in the Medicaid program and the Children’s Health Insurance Program. Bonus payments are specifically given to states that have increased enrollment of qualifying children above baseline enrollment numbers.
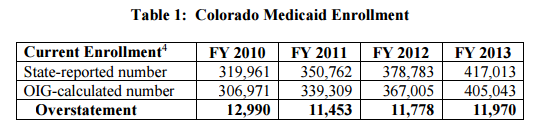
The state of Colorado has shown some discrepancies regarding the number of children enrolled in their Medicaid program when requesting bonus payments when compared to the Medicaid Statistical Information System operated by the Centers for Medicare & Medicaid Services (CMS).
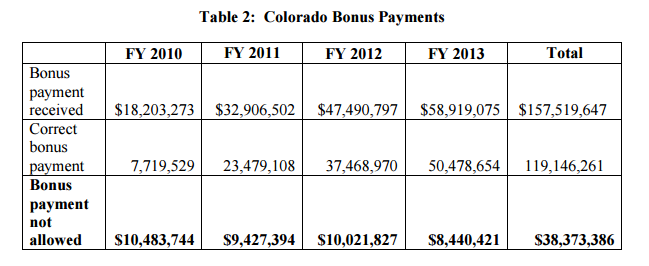
The total amount Colorado received in bonus payments for the fiscal years audited is $157,519,647. The Office of the Inspector General went forward with determining what part of this amount was allowable.
The report does determine that most of the data used by the state of Colorado was in accordance with the law. However, since the state did mislead by overinflating the number of enrolled children in the Medicaid Program, the federal government technically overpaid Colorado in bonus payments under CHIPRA.
Colorado received $38,373,386 in bonus payments that the state was not eligible for. In order to rectify this, the report suggests that Colorado should pay back CMS more than $38 million due to the ineligible bonus payment.
The agency running the Colorado Medicaid program claimed that it has been in full compliance of a CMS guidance from 2009 and the CHIPRA bonus payment program. The state agency also explained that it had followed the federal definition of children to qualify for the program by including blind and disabled offspring.
The Colorado Medicaid Program requested for the Office of the Inspector General to reconsider their findings due to these claims, but the report states that the federal agency maintains accuracy in its auditing processes.
“We disagree that the State agency complied with the Federal requirements for the CHIPRA bonus payments when it included individuals with a BOE code other than 4, 6, and 8 in its current enrollment. The State agency’s current enrollment calculations did not follow the same logic and basis that CMS used to develop Colorado’s baseline enrollment,” the report authors wrote. “As a result, the State agency’s approach overstated Colorado’s current enrollment because it included enrollment categories not reflected in CMS’s calculation of Colorado’s baseline enrollment. Allowing the State agency to include individuals from other BOE categories in its current enrollment counts, when those same BOE categories were not included in the baseline calculations, would result in an artificially inflated estimate of growth in children enrolled in the State’s Medicaid program.”
The report from the Office of the Inspector General included tables that outline exactly how much Colorado’s Medicaid program overstated its enrollment numbers and how many bonus payments should not have been allowed under CHIPRA. Every year from 2010 to 2013, the agency overstated enrollment numbers by more than 11,000 children, which totaled more than $38 million in overpayments over three years.
Ever since the Patient Protection and Affordable Care Act was passed, more than half of all states have gone forward with expanding their Medicaid programs with most of the funding being passed on from the federal government to individual states.
Hospitals and healthcare providers would be the first to benefit from Medicaid expansion. Research shows that states that have expanded their Medicaid Programs have reduced the rates of uncompensated care among hospitals and improved the hospital revenue cycle. On the other hand, regions that have declined Medicaid expansion see a revenue loss among hospitals.
“Ascension hospitals in Medicaid expansion states saw increased Medicaid discharges, increased Medicaid revenue, and decreased cost of care for the poor, while hospitals in non-expansion states saw a very small increase in Medicaid discharges, a decline in Medicaid revenue, and growth in cost of care to the poor. These data suggest that Medicaid expansion can offset the cost of care to the poor and serve as a growing source of revenue as hospitals face cuts in payment and DSH funds,” a report from the Henry J. Kaiser Family Foundation stated.
In the near future, more states may begin expanding their Medicaid programs and the federal government will have more healthcare coverage options to support. It is likely that the Office of the Inspector General will have its hands busy over the coming years when it comes to managing the payment accuracies and auditing processes of state Medicaid programs and the Children’s Health Insurance Program.
Image Credits: Office of the Inspector General
Dig Deeper:
Kentucky Governor Proposes Waiver for Medicaid Expansion
Payment Reforms in NY Medicaid Program Face Challenges