Patient Engagement Cuts Healthcare Spending among Payers
Effective patient engagement solutions, consequently, benefit the health payer industry by reducing healthcare costs.

- Within both federal and state health insurance exchanges, payers are seeking methods for reducing cost in order to avoid profit loss and dropping out of the exchanges much like UnitedHealthcare’s move away from the marketplace. One method for cutting costs seems to revolve around patient engagement and inspiring consumers to change unhealthy behaviors as a method for improving rate of certain medical conditions like diabetes.

Patient engagement can also lead to timely cancer screenings, necessary immunizations, and general check-ups to ensure consumers are on top of their health. Greater patient engagement including beneficiary incentives can lead to an increase in physical fitness and a focus on nutrition as well.
Advancing the patient experience
Patient portals and immediate access to personal health information is also a recommended method for improving engagement and lowering healthcare costs for both providers and payers. The information technology company Optum is looking to improve the patient experience on the insurance side by working with the health information network Availity to bring greater accuracy to medical insurance claims and, thereby, decrease the number of appeals, according to a company press release.
“Availity offers a single point of engagement for health plans and care providers, which leads to improved payment turnaround and more accurate claims submissions. We are delighted to have been selected by Optum to connect its industry-leading ACE solution to our broad national network of health plans,” Russ Thomas, CEO of Availity, said in a public statement.
The solution these companies are working on will bring clear notifications to providers to fix errors and lack of information in order to prevent claims denials. Essentially, this is expected to also boost the patient experience by minimizing payment problems.
“By streamlining the claims process for health plans and care providers, ACE can take unnecessary cost and friction out of the health system, while improving patient experiences,” Bill Miller, CEO of OptumInsight, stated in the press release.
Public and private payers investing in IT systems
When it comes to strengthening health information technology, both private payers on the health insurance exchanges as well as public programs like Medicaid are looking to invest in boosting their IT systems. The Centers for Medicare & Medicaid Services (CMS) reported earlier this month that its annual investment in state Medicaid information technology is more than $5 billion.
Medicaid IT systems need to evolve in order to meet the needs of both healthcare providers as well as beneficiaries. CMS has set up regulations meant to stimulate states to innovate their Medicaid IT systems and follow industry practices.
CMS is looking to move financial incentives from tailor solutions or “custom development” toward small-to-medium-sized vendors in order to create systems and health information exchange solutions that span across state borders. The federal agency even launched a new Medicaid program resource to facilitate these developments.
“Medicaid and the Children’s Health Insurance Program (CHIP) provide health coverage to nearly 72 million Americans, and are consistently growing as more states choose to expand coverage. With over 30 states currently redesigning their Medicaid eligibility and/or claims processing and information retrieval systems, 2016 will the most active year to date for Medicaid growth and new IT business prospects. CMS and states want to make the most of this opportunity,” CMS stated.
“The Medicaid program is undergoing tremendous change, such as a growing emphasis on managed care, offering home and community-based services to seniors and people with disabilities, and developing new models of delivery system reform to improve health outcomes while controlling costs. State Medicaid agencies are hungry for innovation and have pioneered new IT adoption. They were early adopters of Health Information Technology and have issued more than $10.2 billion in incentive payments to providers for adopted and meaningfully used electronic health records.”
Stronger health information exchange will benefit payers, providers, and the patients themselves. Having greater access to personal medical data and electronic patient records benefits consumers by boosting engagement.
How patient engagement cuts costs
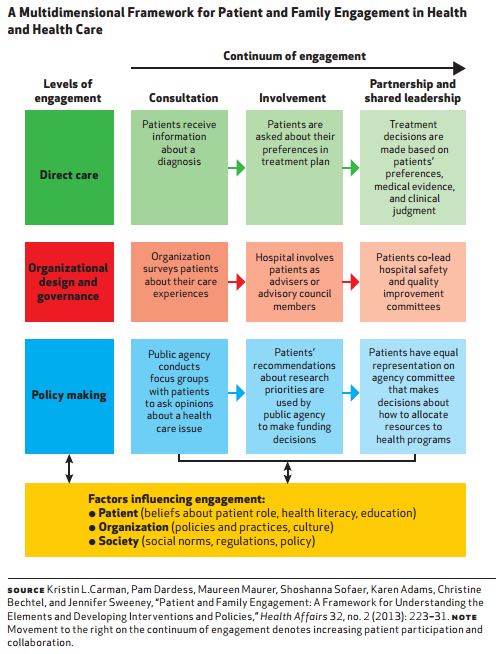
Effective patient engagement solutions, consequently, benefit the health payer industry by reducing healthcare costs. A brief from Health Affairs and the Robert Wood Johnson Foundation elucidates that greater patient involvement in their own medical care brings better health outcomes and decreased healthcare spending.
More healthcare organizations are working toward increasing patient engagement through greater education and by making joint decisions with regard to treatment. Payers would benefit by including these type of hospitals and clinics in their provider networks.
Bringing more healthy patient behaviors to the table is vital in the payer industry’s efforts to cut costs. For instance, patients who seek preventive care and exercise regularly are less likely to be diagnosed with late-stage disease.
The lack of health literacy is still a problem in today’s society and many physicians are still not providing patients with the information they need to make sound decisions about their medical care, the brief explains.
However, shared decision-making and patient engagement is gaining a greater stronghold among the provider community. The brief also discusses the importance of including patient engagement when it comes to end-of-life care. Doctors should communicate with elderly patients about their preferences on end-of-life decisions.
“The Conversation Project, initiated by Boston-based journalist Ellen Goodman and colleagues, is a grassroots public campaign that encourages people to think about how they want to spend their last days and to have open and honest discussions with their families and health care providers,” the brief from the Robert Wood Johnson Foundation stated.
“By having these important conversations before a crisis occurs, patients can consider and clearly communicate their wishes and forestall situations in which those decisions are made by others and not fully aware.”
Additionally, providing consumers with complete and accurate medical information is a key part of strengthening patient engagement initiatives. Many payers have also moved toward integrating beneficiary incentives as a method for reducing the impact of severe medical conditions and, thereby, lowering cost.