Price of Insulin Doubles, Increasing Spending for Members, Payers
The price of insulin has skyrocketed for members and payers, prompting advocates to demand accountability from industry leaders.

Source: Thinkstock
- Dramatic increases in the price of insulin are driving a rapid uptick in overall spending for diabetes care, according to new data from the Health Care Cost Institute (HCCI).
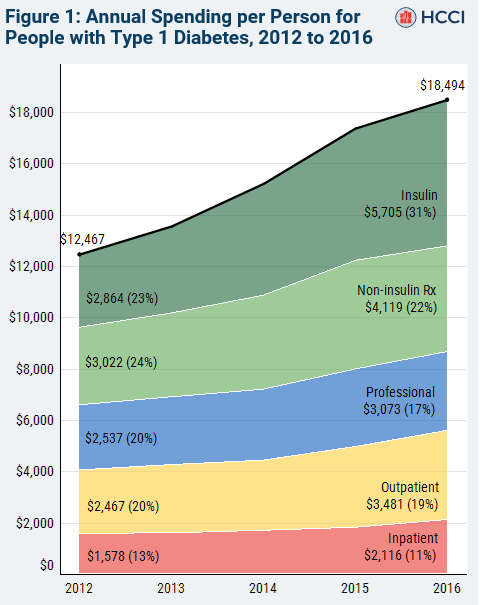
Between 2012 and 2016, the point of sale price for insulin approximately doubled, driving average annual spending for a Type 1 diabetic from $12,467 to $18,494.
Overall use of insulin products remained relatively constant throughout the time period, but the daily expense of being a typical insulin user increased from $7.80 a day in 2012 to $15.00 per day in 2016.
In 2016, gross spending on insulin accounted for more than 30 percent of the total annual spending on diabetes care, with similar prices across the different delivery mechanisms for basal insulin and mealtime insulin.
HCCI does not have access to proprietary payer information on rebates and coupons, and the report acknowledges that these benefits may have increased for consumers alongside the overall price of these products.
However, even with assumed rebates of 50 percent, out-of-pocket spending still increased significantly.
“The net increase in total spending per person would be $4,606, reflecting a $1,421 increase in spending on insulin,” the report states.
“Increased spending on insulin net of rebates and coupons would account for 31 percent of the total increase in spending and would still be the category with the largest increase. On net, the average price of insulin would still have doubled between 2012 and 2016.”
The price spikes have attracted national attention over the past few years, prompting lawmakers and industry observers to question the reasoning behind the steady climb.
Source: HCCI
Major news outlets have reported on deaths due to lack of access or rationing of high-cost insulin and widespread consumer confusion about steep upticks in their prescription bills.
In January, the House Oversight Committee launched an investigation into skyrocketing drug prices, noting that a recent Inspector General report found a 62 percent increase in Medicare Part D payment for name-brand drugs between 2011 and 2015, despite a 17 percent decrease in the number of prescriptions written.
“The Committee on Oversight and Reform is investigating the actions of drug companies in raising prescription drug prices in the United States, as well as the effects of these actions on federal and state budgets and on American families,” said Committee Chairman Rep. Elijah E. Cummings (D-MD).
“For years, drug companies have been aggressively increasing prices on existing drugs and setting higher launch prices for new drugs while recording windfall profits. The goals of this investigation are to determine why drug companies are increasing prices so dramatically, how drug companies are using the proceeds, and what steps can be taken to reduce prescription drug prices.”
Several varieties of insulin from multiple manufacturers are among the drugs under scrutiny.
Insulin is not the only drug under investigation, but with close to 10 percent of the US population living with diabetes, the impacts of unaffordability are stark and wide-ranging.
The American Diabetes Association (ADA) has collected nearly half a million signatures on a public petition stating that “insulin is not a luxury” and urging lawmakers and drug companies to address inflated prices.
In 2016, the association launched the Make Insulin Affordable initiative to educate the public and advocate for pricing controls.
“There is no substitute for insulin, and access to insulin is a matter of life and death for more than 7.5 million Americans with type 1 and type 2 diabetes,” said Chief Scientific, Medical, and Mission Officer William T. Cefalu, MD, in 2018.
“Too many are faced with the unacceptable choice of either rationing or forgoing insulin doses to reduce out-of-pocket costs, despite the serious and potential deadly complications of improper insulin dosing.”
The initiative’s website includes resources for individuals struggling to pay for their necessary medications.
Drug manufacturers are currently taking most of the heat for pricing issues, but insurance companies and pharmacy benefit managers also have a responsibility to control the market – not to mention a financial stake in the matter.
Ensuring that chronic disease patients have continuous and affordable access to insulin is a preventive measure that can trim hospital costs down the line and increase member loyalty.
Putting pressure on manufacturers and supporting federal and local efforts to curb price increases may have positive impacts on consumer perception and the likelihood that members will retain coverage that offers them affordability and advocacy.
