Risk-Stratified Care Management Enables Customized Treatment
The goals of risk-stratified care management programs is to prevent chronic diseases among patients and ensure the best health among the consumer base.

- Among health payers, one necessary strategy aimed at ensuring superior patient health outcomes is based on risk stratification and the data analytics behind this process. The American Academy of American Physicians defines risk-stratified care management as a method for assigning patients a health risk category and using the information to better improve care and tailor treatments and services based on each patient’s needs.

The goals of risk-stratified care management programs is to prevent chronic diseases among patients and ensure the best health among the consumer base. For instance, keeping patients at risk of more serious conditions at a more stable level and halting the progression of a disease while keeping costs low are some of the positioned outcomes of risk-stratified care management.
The first step is to identify the risk category that a patient falls into. Then a medical team can work toward developing a customized treatment plan along with the collaboration of the patient. This may include a variety of resources from community assistance to better care coordination among multiple medical teams or intensive care management.
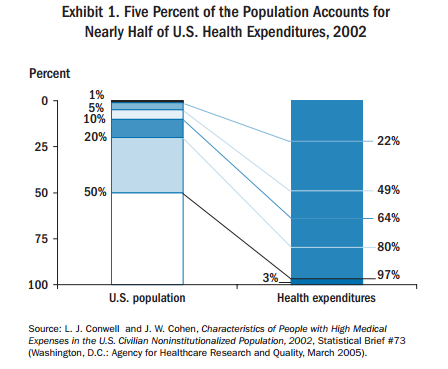
Risk-stratified care management could be vital for the data analytics behind medical services. For example, as many as 200 patients out of a total of 1000 would benefit from more intensive support and care. Additionally, this 20 percent of the patient population actually takes up 80 percent of total medical spending, according to a brief issued by the Commonwealth Fund.
Payers and providers who utilize risk-stratified care management programs can actually benefit in the ongoing healthcare payment reforms taking place around the nation. A medical practice would be better prepared for any changes taking place throughout the industry when utilizing risk stratification.
Changing payment models will likely include population health measures in future versions, which will rely on risk stratification as well. Reimbursement will depend upon the additional resources and healthcare services necessary to manage populations at higher risk of certain medical conditions or generally in need of more medical support.
The Commonwealth Fund brief outlines the importance of risk-stratified care management, which includes a method for balancing the insurance market more effectively. For example, it allows for subsidizing insurers who have the majority of their consumer base exhibiting higher than average medical costs when compared to insurers “with a better selection of health risks.”
“The Affordable Care Act takes several steps to mitigate risk selection. Except for grandfathered plans, it requires insurers in the individual and small-group markets to offer similar sets of essential benefits. The Act also requires insurers to charge their individual or small-group subscribers the same rates regardless of whether the coverage is sold through the new insurance exchanges or regular insurance markets,” the brief stated.
“Finally, subscribers who want to receive premium subsidies or tax credits must purchase through the exchanges. These and other measures (such as limited open enrollment periods) will reduce some risk skewing but will not eliminate all potential risk-selection problems. Realizing this, Congress created three specific mechanisms—risk adjustment, risk corridors, and reinsurance—to mitigate insurer risk and to reduce incentives for risk selection under the market structures.”
The American Journal of Managed Care published a study in which researchers attempted to identify through risk stratification what type of patients would benefit the most from greater care coordination and a patient-centered medical home model of care.
The study used retrospective cohort analysis when it came to the data analysis aspect of the research. Seven models of care were used to find which patients benefit the most from the patient-centered medical home. These models include Adjusted Clinical Groups (ACGs), Hierarchical Condition Categories (HCCs), Elder Risk Assessment, Chronic Comorbidity Count, Charlson Comorbidity Index, and Minnesota Health Care Home Tiering as well as a combination of Minnesota Tiering with the ERA score.
There are a wide variety of data sets that were looked at when determining patient risk such as the number of emergency room visits, hospitalizations, and readmission rates within a 30-day timeframe.
The researchers essentially wanted to see which risk stratification care management method was best out of the seven models when it comes to predicting the patients that need the greatest care coordination. The results show that the Adjusted Clinical Groups (ACGs) model performed best and was able to effectively predict the top 10 percent of highest cost users.
This type of study is very beneficial for both providers and payers to comprehend. Knowing the best model for risk stratification data analysis could position the healthcare industry to provide quality, coordinated care at reduced costs. As previously stated, preventing disease and tailoring treatment could lead to better care, fewer emergency room visits, and thereby lower spending.
“We assessed 6 risk instrument methods based on administrative and demographic data,” the researchers wrote in the published paper. “We evaluated the performance of the 6 models against one another to assess the ability to predict future healthcare utilization. We concluded that the ACGs produced a more accurate prediction of future healthcare utilization relative to the other models.”
