Total Medicaid Expansion May Cut Uninsurance, Uncompensated Care
Researchers analyzed the potential effects of total Medicaid expansion and found that it could lead to 28% lower uninsurance and less uncompensated care.
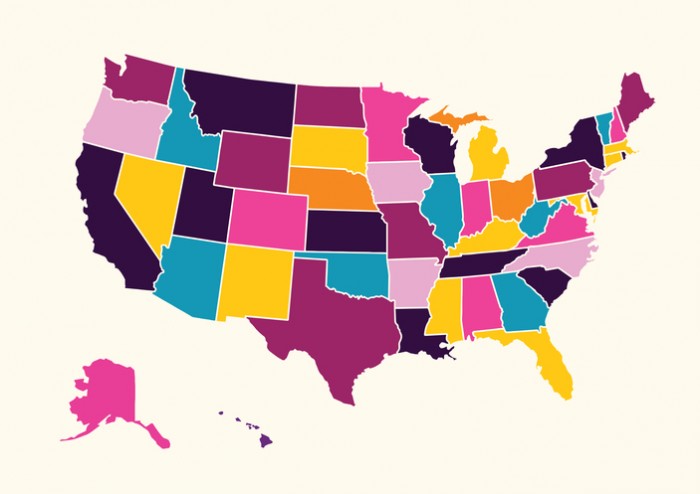
Source: Thinkstock
- If all of the nonexpansion states adopted Medicaid expansion, thus establishing total Medicaid expansion nationwide, there would be a 28 percent reduction in uninsurance, the Urban Institute found in its report which HealthPayerIntelligence received via email.
Using the Health Insurance Policy Simulation Model (HIPSM) and data from 2017 through 2020, the researchers gauged what Medicaid enrollment might look like if the 15 nonexpansion states were to adopt Medicaid expansion.
The report estimated Medicaid costs using the 2014 through 2016 Medicaid Statistical Information System and data along with recent state data. The model assumes similar uptake across all of the states and does not take into account many of the impacts of COVID-19 for which data is not yet available.
In addition to 3.9 million fewer uninsured Americans, 6.5 million people would gain Medicaid coverage and 185,000 people would transition from short-term limited-duration plans, which have received criticism, to health plans that meet the Affordable Care Act’s quality standards. The researchers also anticipated that around 1.4 million would transition from subsidized marketplace plans to Medicaid.
The number of those without an assistance option would drop by almost four million from 9.3 million to 5.4 million. Meanwhile, each of the 15 states would see an increase of or above 25 percent, with the exceptions of Wisconsin and Tennessee.
If the pandemic had not happened, the model found that uninsurance among the nonelderly would be around 14.5 percent. If all 15 states implemented Medicaid expansion, the uinsurance rate would fall about four percentage points down to 10.4 percent. Three states would have 12 percent or more uninsurance, but five of the 15 would have eight percent or less uninsurance.
Federal healthcare spending on Children’s Health Insurance Program (CHIP), marketplace subsidies. States that could experience significantly higher federal income usually have:
- Lower-than-average eligibility determinants for parents than most states
- Lower ACA marketplace enrollment
- Higher uninsurance
Without the pandemic, other federal spending in current nonexpansion state Medicaid programs would have risen by around $30.4 billion.
State spending would rise by a little over nine percent (around $4.7 billion). Normally, states would spend $51.6 billion.
But the states would also experience savings that could leave states a net positive budget. For example, the states would face far less in uncompensated costs: through Medicaid expansion, uncompensated care demand would have dropped by about $6.4 billion total for the 15 nonexpansion states. That could save the federal government $2.6 billion and states and local governments $1.6 billion, and providers could save $2.3 billion.
Financial benefits are not the only advantage to Medicaid expansion, according to the Urban Institute.
“In addition to reducing the number of uninsured, expanding Medicaid under the ACA to low-income people improves health and reduces mortality in the enrolled population,” the researchers noted.
Previous studies by the Kaiser Family Foundation, Urban Institute, Health Affairs, and the Yale Cancer Center have brought to light multiple potential benefits of Medicaid expansion including that Medicaid expansion:
- May help the economy
- May lower uninsurance
- May improve patient outcomes
- May close racial gaps in care disparities
The researchers found that these added benefits and others could save expansion states money through increased tax revenue from increased economic activity, increased state provider tax and premium revenue, and lower demand for state-funded programs for uninsured and low-income Americans.
“Most states with relevant analyses expect net fiscal gains, even after states begin paying 10 percent of expansion costs,” the researchers said of the current states with Medicaid expansion, expecting that this trend would be the same for nonexpansion states if they transitioned as well.
And while there are many uncertainties to account for in a study that attempts to project coronavirus-related circumstances, the researchers found that, in some ways, lessons from the COVID-19 pandemic only fortified their findings.
“The current situation highlights the more robust safety net in place for those facing crisis circumstances in states that have implemented Medicaid expansions,” the researchers concluded.
