Why Bundled Payments Are a Popular Option for Healthcare Payers
Bundled payments present payers with a low-risk way to manage healthcare payments, increase care quality, and participate with providers in value-based care.
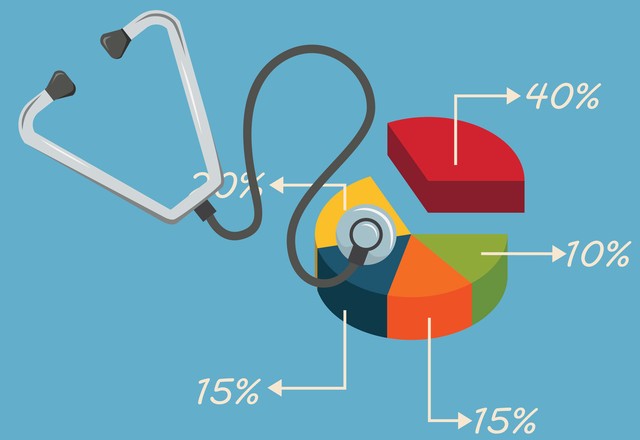
Source: Thinkstock
- Bundled payments are ideal for payers that want to participate in value-based care. Bundled payments tend to have lower financial risks than other payment models for payers and are beneficial to providers as well as payers.
In a bundled payment arrangement, payers are only responsible for a single payment that covers all the services included in a defined episode of care, which means there is lower financial risk than other types of value-based agreements for payers. Bundled payments can be administered as one bulk payment to a provider organization, or dividend payments to participating providers, making it easier for payers to manage reimbursement totals.
Payers have a growing base of providers ready to participate in bundled payment models. CMS reported a six percent increase in the use of alternative payment models in 2016. Twenty-nine percent of healthcare payments made in 2016 were under a bundled payment model, shared savings payment model, or a similar alternative payment model.
Bundled payment models remain a popular reimbursement option for payers because of opportunities to increase care quality, decrease care costs, and manage high healthcare spending. Leading payers experts have identified bundled payment models as a way for payers to effectively define their total costs of care.
Bundled payments help produce payer and provider cost savings
Bundled payments have linked to improvements in healthcare cost savings for both payer and provider organizations, which may incentivize both groups to participate in bundled payment models.
READ MORE: How Payer Philanthropy Can Address Social Determinants of Health
Research from the Altarum Institute found that joint replacement bundled payments can lower costs without sacrificing patient volume or quality.
The team found that hospitals participating in the Bundled Payments for Care Improvement (BPCI) initiative under CMS reduced costs by $3,286. Non-participating hospitals reduced mean Medicare reimbursements by $2,119. The bundled payments analyzed in the study also did not sacrifice quality of care for cost-savings.
Employer-sponsored health plans can also leverage bundled payments to reduce costs, according to the DRIVE Health Initative. DRIVE found that bundled payment amounts were 10 to 12 percent lower than fee-for-service amounts for certain surgical procedures. Larger employers that cover thousands of employees, such as Walmart, Lowe’s, JetBlue, and McKesson, were able to use bundled payments to reimburse surgical services at lower rates.
Bundled payments could assist in population health management and healthcare spending amounts
Payers can leverage population health management techniques and value-based insurance design to treat high-risk, high-cost individuals. A bundled payment model could allow a payer to bundle payments for multiple services in population health programs in years to come, according to an analysis of bundled payments published in JAMA.
The next generation of bundled payments could facilitate population health programs with longer treatment periods to address all of the conditions of high-risk populations, and offer more diverse bundled payment types beyond popular joint replacement models.
READ MORE: How Provider-Sponsored Health Plans Can Find Consumer Success
Combining bundled payments with population health management techniques could assist payers with the ballooning costs of healthcare in the US.
In 2016, healthcare costs jumped to $3.3 trillion dollars and healthcare spending is expected to grow by 5.4 percent per year from 2016 to 2028. The use cost-effective bundled payments to drive cost-effective population health programs may help payers curb trillions in spending.
Bundled payments are a growing opportunity despite new federal policies
Healthcare experts and payer organizations believe that payers will have an opportunity to succeed in bundled payments, even with federal policy changes involving mandatory bundled payments.
A newly passed CMS final rule eliminated mandatory bundled payments for joint replacements for CMS providers. Providers can still voluntarily accept bundled payments under the new rule. The rule is not expected to drastically affect the rate of payers adopting bundled payment models, according to Colin Luke, a partner at Waller Lansden Dortch and Davis.
“Private payers are going to stay on target with the exception of Medicare Advantage plans, which are much more in sync with Medicare policies,” Luke said.
READ MORE: Member Engagement, Payer Spending Lead Top 10 Stories of 2017
“But with private payers that already have value-based purchasing programs underway, whether they are in a beta phase, a demonstration project or throughout its network, I do not think that these CMS delays and move away from mandatory programs is going to delay that or alter it significantly.”
Bundled payments allow payers to determine their total reimbursement amounts for services, which is especially valuable to employer-sponsored plans. Leaders at DRIVE view bundled payments as a way for payers and employers to define healthcare value in a holistic manner.
“If we can’t measure quality, then we can’t pay for it,” Bill Kramer, MBA, Executive Director of National Health Policy at the Pacific Business Group on Health said. “Bundles total accountability for the total cost and outcome of care from these procedures. We believe it’s a catalyst to transform care throughout the entire [healthcare] system.”
Payers aiming to address the many financial and quality challenges they face when sponsoring health plans could look to bundled payments as a solution to deliver high quality, cost-effective care.
