Why Payers Need Robust Health Information Technology
The loss of private data shows that some insurers may not be fully equipped to incorporate health information technology in a secure manner.

- Health information technology continues to be an elusive field for the payer industry, as some insurers still have difficulty with adhering to key technological advancements and data security protocols. For example, the health insurer Centene announced last week in a press release the loss of six hard drives that containing the personal information of 950,000 individuals.

Data privacy and security missteps
Currently, the organization is conducting an internal search through its health information technology platforms to find the lost files. The data pertains to patients who have received laboratory services over the last six years. In particular, the data contains names, social security numbers, addresses, dates of birth, member ID information, and medical history.
“Centene takes the privacy and security of our members' information seriously,” Michael F. Neidorff, Chairman, President and CEO of Centene, said in a public statement. “While we don't believe this information has been used inappropriately, out of abundance of caution and in transparency, we are disclosing an ongoing search for the hard drives. The drives were a part of a data project using laboratory results to improve the health outcomes of our members.”
“Consistent with our policies around communication and transparency, we are beginning the process of notifying all affected individuals and all appropriate regulatory agencies as we continue to search and investigate,” Neidorff concluded.
Mismanaged enrollment processes
Nonetheless, the loss of such private data shows that some insurers may not be fully equipped to incorporate health information technology in a secure manner. Blue Cross and Blue Shield is a major payer across the industry, but seems to have had an onslaught of serious enrollment issues as of late, according to The Charlotte Observer.
The problems stem from customers who can’t make payments and received the incorrect billing information to consumers who enrolled but have no confirmation and some who were signed up for a plan they did not choose. As such, Blue Cross and Blue Shield may benefit from greater investment in their health information technology solutions so that such major issues become a thing of the past.
Currently, Blue Cross and Blue Shield did state having re-established health coverage for thousands of customers that had previously lost their insurance due to these technological mishaps. The North Carolina Attorney General along with the North Carolina Department of Insurance plan to determine what went wrong and what laws could have been violated.
“We do not know the end date for a solution,” Insurance Commissioner Wayne Goodwin told the news source. “It is vital that we address the consumer complaints and policyholder needs first, and then address this crisis from a regulatory standpoint.”
The insurer is located in Chapel Hill and has been inundated with at least 450,000 calls from customers in the first week of January. At this moment in time, however, the Blue Cross chief executive has stated that most problems have been solved and the majority of health insurance cards have been re-sent to pertinent customers.
“I’m encouraged on the progress we are making on our operational issues,” Blue Cross’s Chief Executive Brad Wilson wrote to employees. “We’ve made good strides over the past week, particularly on enrollment, ID cards and incorrect bank drafts.”
The need for health IT solutions
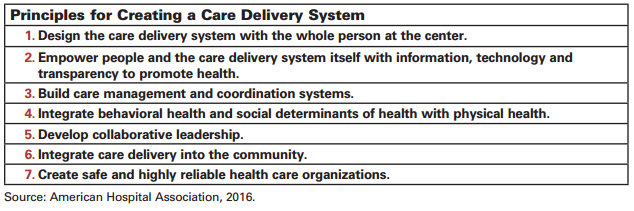
Clearly, more effective and reliable health information technology solutions must be incorporated within the payer industry to avoid these enrollment issues. One report from the American Hospital Association’s Committee on Research and Committee on Performance Improvement emphasizes the need to strengthen the healthcare delivery system with useful information, cost transparency tools, and new technologies.
Health information technology can be used to boost patient engagement with their own health and wellness, which will lead to improved health outcomes and subsequent reduced medical costs. For example, payers can invest in portals and telehealth technology in order to improve patient engagement and lead consumers to make smarter healthcare decisions aimed at cutting overall medical costs.
Payers, providers, government agencies, and the patient community may need to form new partnerships in order to leverage the benefits of technology and improve access to pertinent data. As such, strong health information exchange systems will need to be put in place.
Gregory Barnowsky, Chief Architect at Independence Blue Cross, wrote for the Healthcare Information and Management Systems Society (HIMSS) about some of the key elements needed for successful health information exchange. First, stakeholder needs must be met in an effective manner. Second, it is beneficial to constantly search for certain areas in which health information exchange systems could benefit the patient community and stakeholders.
The last important point for designing a successful health information exchange platform includes finding “new sources of funding” meant to keep the system operational. By incorporating these key points, payers can integrate strong health IT infrastructures and ensure their health information exchange systems are functioning properly. Barnowsky also mentioned the effect of digital disruption on health information exchange.
“Digital disruption around big data, mobile devices, personal and biometric devices, and cloud-based easy access to data sharing all serve to put additional pressure on new and existing HIEs to adopt quickly to change,” Barnowsky wrote. “Most HIEs are initially focused on the interactions from physician, hospital, and even payers with patient as last on the list. However, digital disruption may force HIEs to include patient data sharing earlier in their implementations causing additional planning and effort, data security and costs.”
In order to reduce the potential risk for customer privacy and security violations as well as significant enrollment issues, health payers are encouraged to invest in implementing health IT platforms capable of handling massive amounts of data.