Why Population Health Data is Integral for Value-based Care
Population health data analysis is necessary for providers to meet quality benchmarks as part of value-based reimbursement.

- The study of population health data could be relevant for both payers and providers, as it could affect reimbursement for healthcare services. As hospitals and clinics continue to promote wellness programs, improve patient safety, and reduce hospital readmission rates, the impact on the health of populations is expected to be beneficial.

As providers step away from fee-for-service payment models and adopt value-based care as well as population health management strategies, healthcare costs are expected to fall.
What’s important to keep in mind is that the impact of population health data is dependent on some of the key healthcare reforms taking place throughout the country including greater aim to adopt value-based care initiatives like Accountable Care Organizations and bundled payments. Population health data analysis is necessary for providers to meet quality benchmarks as part of value-based reimbursement.
The Department of Health and Human Services (HHS) announced last year that at least 30 percent of claims received by the Centers for Medicare & Medicaid Services (CMS) will come in the form of alternative payment models starting in 2016. By 2018, it is expected that half of all claims to CMS will be in the form of alternative reimbursement arrangements.
A report from The Academy Huron Institute states that population health management will be vital as more providers switch over to value-based care initiatives and leave fee-for-service payment models in the past. Risk-based arrangements that pay more attention to patient health outcomes and reduced admissions will be a common occurrence throughout the healthcare industry.
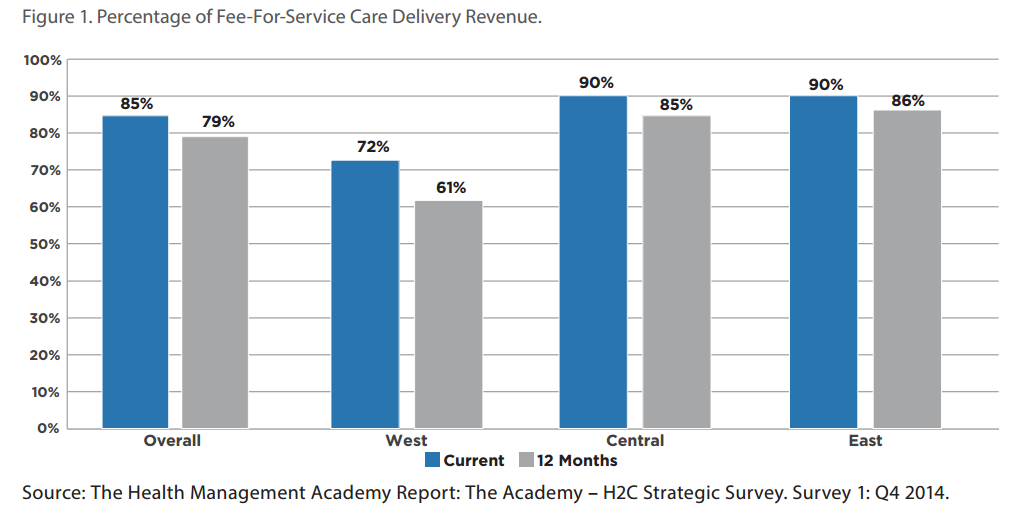
Last year showed a slow transition toward value-based care with 15 percent of healthcare services using these alternative payment models while 85 percent still remained on a fee-for-service program, according to a survey conducted by The Academy Research. The results also show that western parts of the United States have more services tied to value-based care while central and eastern regions of the country are more aligned with fee-for-service.
The report also mentions how a provider-owned health plan could be an avenue for medical facilities to better align themselves with population health management and value-based care.
Survey results show that most hospital systems choose commercial shared savings as a payment model for at-risk revenue. Additionally, bundle payments and partnering with a health plan were some other typical ways to assume at-risk payment models. The use of these value-based care and alternative payment models is further pushing forward population health management and the inclusion of patient or consumer engagement in an effort to improve health and wellness among the public.
Patient engagement may be seen in the form of adopting patient portals and providing access to personal electronic medical records. Additionally, greater patient support and superior scheduling services can assist in promoting consumer engagement.
The report from The Academy Huron Institute also showed that healthcare providers are putting more of their budget toward investments in population health management strategies. This means that risk and value-based care will take a stronghold throughout the healthcare industry over the coming years. There are three main takeaways from the Huron Institute’s report.
“First, there is a steady and deliberate shift in the market toward the assumption of risk and the development of risk-based programs. While the appropriateness of the rate of change can be debated, health systems can be sure that transformation has started and population health management is the future of healthcare delivery,” according to the report.
“Second, health systems are making an organizational commitment to population health by increasing budgets, building strategic priorities, evolving payer relationships, and creating new ways of paying caregivers all in the interest of advancing population health. Third, health systems continue to make developments in infrastructure to manage risk with strong enterprise leadership and cultures for advanced analytics.”
The American Health Information Management Association (AHIMA) stated that the aim of population health management is to keep patients as healthy as possible with preventive strategies and keep patients with chronic conditions from becoming more ill. These methods of care are expected to keep costs low.
It is also essential to understand that the analysis of population health data is composed of studying the financial and clinical risk among a certain group of patients. When creating a population health management program, it is vital to determine which metrics to measure and how both financial and clinical risk will be analyzed.
A typical population health management program also brings focus to tracking the number of patients taking part in emergency room visits, hospital admissions, and ambulatory services.
The collection of population health data will involve reporting any healthcare gaps as well as alerting physicians to any patient needs. Automation software can be used to collect population health data and alert care managers about any type of support a patient may require.
“We are beginning to see tremendous pull through from patients, clinicians and hospitals for the kinds of rich informatics and insights enabled by open solutions geared toward keeping patients healthy and reducing overall cost,” Allscripts President and Chief Executive Officer Paul Black stated in a press release.
“Population Health Management can be viewed in three dimensions: enabling innovation and technology solutions on an open, community-wide platform, partnering with clients to ensure rapid adoption, and supporting the fundamental redesign in care enabled by Population Health Management.”