An Overview of the CMS AHEAD Model for Health Equity Advancement
Participating states could receive as much as $12 million through the AHEAD model to align various payers on health equity goals.

Source: Getty Images
- The CMS States Advancing All-Payer Health Equity Approaches and Development Model (AHEAD Model) rallies states and a broad scope of healthcare stakeholders around health equity improvement through primary care investments and global hospital budgets.
“In our current health care system, fragmented care contributes to persistent, widening health disparities in underserved populations,” CMS Administrator Chiquita Brooks-LaSure said in the press release. “The AHEAD Model is a critical step towards addressing disparities in both health care and health equity while improving overall population health.”
Eight states will leverage millions of dollars from CMS to improve health equity for their beneficiaries. The model employs a total cost-of-care approach.
CMS has supported models like the AHEAD model in the past. Examples include the Maryland Total Cost of Care Model (MD TCOC), the Pennsylvania Rural Health Model (PARHM), and the Vermont All-Payer Accountable Care Organization (VT ACO) Model. However, unlike these models, AHEAD will apply these strategies in more than one state simultaneously.
Source: CMS
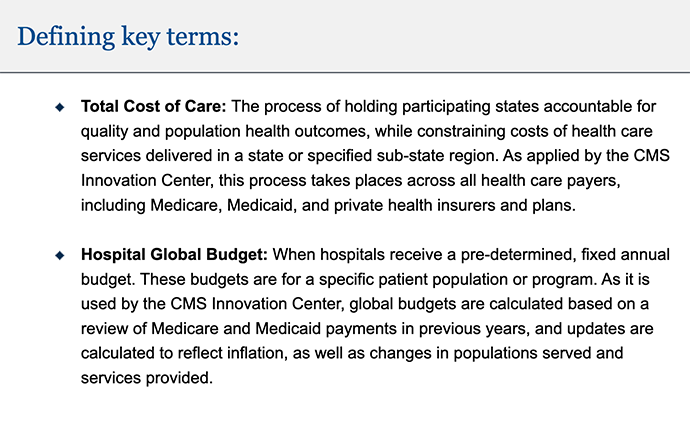
What is the model?
Model components
The AHEAD model takes the total cost of care model and enacts it across multiple states. CMS will offer support for primary care, hospital global budgets, and community resources alignment, the agency summarized in a LinkedIn post.
CMS will work with participants to set a Medicare total cost of care growth target. States will establish their own all-payer cost growth targets. Additionally, states will have all-payer and Medicare primary care investment targets.
Participating states will leverage funding for primary care services to facilitate multi-payer primary care transformation. This effort will involve higher traditional Medicare investment and aligning strategies for advanced primary care in traditional Medicare and Medicaid.
For the primary care portion of the model, payers can receive the Medicare Enhanced Primary Care Payment (EPCP) on a quarterly, prospective basis. CMS apportions the payment per beneficiary. Quality performance will impact some aspects of the payment.
There are three categories of primary care transformation requirements. Participants must demonstrate behavioral health integration, health-related social needs, and care management and specialty coordination.
States can also implement hospital global budgets, including incentive payments, to improve care design for Medicare and Medicaid beneficiaries.
Participants receive these payments as an annual budget. CMS calculates the budget using past Medicare and Medicaid payments with accommodations for inflation and changes in population or services. States can set their own hospital global budget methodology or leverage the CMS Medicare fee-for-service global budget methodology with certain specifications based on provider type.
The hospital global budgets and primary care investments will involve social risk adjustments and bonuses for hospitals that improve their care disparity quality measures.
Non-Medicare or -Medicaid payers can be involved in the model’s primary care transformation and hospital global budget goals. They can participate by providing prospective care management payments and employing global hospital budgets based on targeted patient populations.
Beyond financial support, the model will improve care coordination to reduce care disparities. Additionally, model participants will seek to strengthen Medicare and Medicaid beneficiaries’ preventive care through community partnerships and screenings.
In order to support health equity advancement, states must participate in a statewide health equity plan and a statewide, cross-sector model. Hospitals also must formulate a health equity plan that coincides with the state’s goals. Providers will use health-related social needs screenings and collect demographic data.
Participants will receive, at most, $12 million through an initial award and non-competing annual awards.
“Primary care is the foundation of a high-performing health system and essential to improving health outcomes for patients and lowering health care costs. For that reason, the CMS Innovation Center has invested significant time and resources over the years testing models to strengthen primary care and improve care coordination and linkages to organizations that address health-related social needs,” Deputy CMS Administrator and Innovation Center Director Liz Fowler noted in the press release.
“Through AHEAD, more states will have the exciting opportunity to both improve the overall health of their population, support primary care, and transform health care in their communities.”
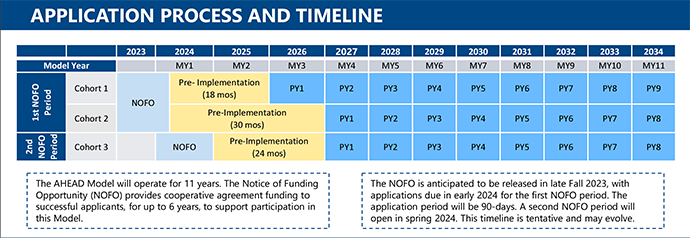
Model timeline
The model will run for 11 years. The agency releases the first of two notices of funding opportunities in the autumn of 2023, and states will have 90 days to apply. After that, the application period will run in the spring of 2024. The second notice of funding opportunity will occur in the spring of 2024 and close after 60 days. The model will end in December 2034.
However, participants’ actual start and end dates will depend on their chosen cohort.
The model will involve three cohorts. States will apply to a cohort based on their preparedness. The first cohort is for states prepared to put their plan into action immediately, whereas the third cohort is for states still waiting to be ready to implement their models.
Cohort 1’s pre-implementation period will tentatively last from July 2024 to December 2025. Its first performance year will be in January 2026.
Cohort 2 will have a pre-implementation period of 30 months, stretching from July 2024 to December 2026. The first performance year will start in 2027. This extended pre-implementation period will give the cohort extra time to prepare the remaining facets of their models that still need to be prepared when the model begins.
Cohort 3 will start its pre-implementation period in January 2025 and continue through December 2026. Its first performance year is set potentially for 2027.
Source: CMS
Eligibility
CMS anticipated awarding funding to as many as eight states in total. Participating states must have at least 10,000 Medicare fee-for-service Part A and Part B beneficiaries in the state or sub-region, according to the fact sheet.
State agencies can apply for this funding opportunity if they can contract with the HHS Secretary for their states. Potential awardees include state public health agencies, state insurance agencies, or state Medicaid agencies.
Additionally, hospitals, health systems, and primary care providers in participating states can engage in this model. Acute care hospitals, critical access hospitals, and rural emergency hospitals—with specific qualifications—are eligible for the Medicare fee-for-service global budget.
Why did CMS introduce this model?
The agency expressed that this model would keep states accountable for healthcare spending in Medicare and across all payers. Additionally, the model emphasizes improvements in primary care, health equity, and population health.
The primary care portion of this model has multiple goals. First, it seeks to boost primary care investment. It also aims to align payers on primary care efforts, improve uptake of advanced primary care, and recruit more providers, including safety net and rural providers.
The hospital global budgets segment of the AHEAD model seeks to reduce unnecessary care and increase care coordination. Additionally, providers will seek to improve health outcomes.
States that want to participate in the AHEAD model can submit their applications through grants.gov. They may also subscribe to the model’s listserv.
