Medicaid Spending Drops When Members Transition to Community Care
Medicaid spending decreased when members transitioned from long-term institutional care into community care settings, a new report finds.

Source: Thinkstock
- Medicaid spending declined when beneficiaries transitioned from long-term institutional care into community care, a new report conducted by Mathematica Health Policy found.
Researchers observed cost outcomes of Medicaid’s Money Follows the Person (MFP) demonstration, which began in 2008 to provide financing to help state Medicaid programs move beneficiaries from long-term support service (LTSS) institutions into apartments, houses, or group homes.
“LTSS users account for 6.4 percent of the Medicaid population, but for 45.6 percent of Medicaid expenditures,” the team explained. “As of fiscal year 2010, Medicaid spent approximately $35,000 on LTSS (institutional and community services combined) per beneficiary, and another $7,000 on non-LTSS expenditures.”
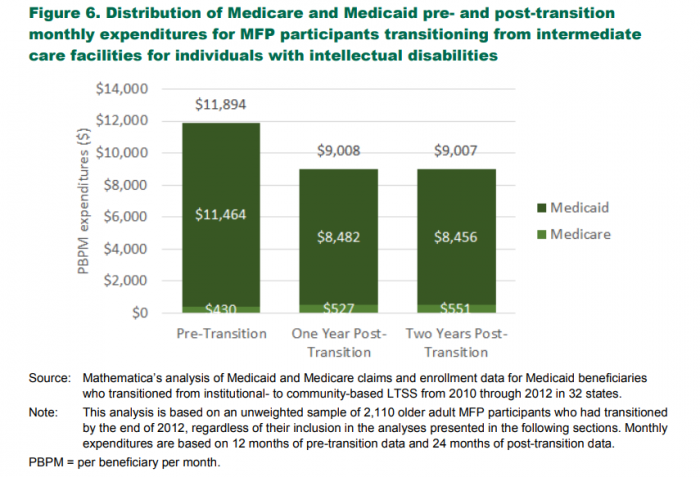
During the first two years of the demonstration, average per-month spending for MFP beneficiaries decreased from $3865 to $2723 on the lower end of spending, and $11,367 to just over $8000 on the higher end of the scale.
Medicaid spending for adult populations above the age of 65 declined by 20 percent in the MFP’s first year and by 27 percent in the second year.
Source: Mathematica Health Policy
Healthcare expenditures for MFP beneficiaries averaged $7892 per month, with institutional care expenses accounting for nearly $4000 of total spending.
The first year of the MFP led to a decrease in average monthly expenses of $6351 per member. The second year continued to lower costs, producing monthly beneficiary costs that averaged $5751 per member.
Institutional care costs steadily dropped as MFP participants moved out of institutional care into community settings. These costs fell $607 per beneficiary in the MFP’s first year and jumped to $1094 per member in year two.
Costs for community-based LTSS increased as more beneficiaries transitioned out of long-term institutions. First-year community LTSS monthly expenses reached $2742 per beneficiary but decreased to $1751 per member in the MFP’s second year.
In addition, MFP beneficiary costs also shrank within inpatient facilities, skilled nursing facilities, and other healthcare settings.
The researchers pointed out that the care costs of MFP members were higher than costs for other Medicaid beneficiaries that transitioned out of institutional LTSS settings. MFP beneficiaries over the age of 65 or those who had developmental disabilities cost upwards of $2000 more than non-MFP members.
“MFP participants had considerably greater LTSS expenditures during the first year after the transition because they received more community-based LTSS, which was by design,” the team said. “During the second year, total monthly expenditures for MFP participants were only marginally greater than those of the matched other transitioners.”
The team argued that the MFP member population were more vulnerable than non-MFP groups. MFP beneficiaries were also more likely to have lingering high healthcare costs during post-transition periods outside of institutional care.
Future developments of the MFP may require more analysis of the relationship between reductions in Medicaid spending and healthcare outcomes, the team asserted.
Reducing Medicaid spending may increase unmet care needs for beneficiaries that are available in long-term institutional care. Additional analysis should help determine if community-based LTSS can adequately meet healthcare needs for beneficiaries.
“Lower or declining expenditures are not always desirable, especially if they represent an increase in unmet need,” the team said. “In the case of MFP, declines in spending on community-based LTSS were by design and do not seem to have come at the detriment of increased medical spending or institutionalization.”
“On average, when Medicaid beneficiaries transition from a long institutional stay to community-based LTSS, their total Medicaid and Medicare expenditures decline,” the team continued.
“This decline in expenditures occurs whether or not the beneficiary participates in the MFP demonstration, as reflected by the comparison between MFP participants and other beneficiaries who experience the same transition without the benefits of the MFP demonstration.”
