Top 3 Ways to Meet HEDIS Quality Measures, Improve Performance
Currently, more than 90 percent of health plans use HEDIS to determine their overall performance when it comes to serving their consumer base.

- The entire healthcare industry benefits greatly from the quality measurement programs including the Healthcare Effectiveness Data and Information Set (HEDIS) tools developed by the National Committee for Quality Assurance (NCQA). The HEDIS quality measures allow consumers and employers determine the best coverage options and optimal healthcare services.

The quality performance analysis provided by the NCQA allows hospitals, physician practices, and health payers to learn about which areas need improvement and where they are excelling. This will allow these organizations to strengthen their services and coverage plans over time.
Towards that end, we will outline a variety of ways that payers can use HEDIS quality measures to improve their overall performance and ensure superior coverage options among their consumer base.
HEDIS quality measures are one of the most common performance standards among managed care facilities including the Accountable Care Organization (ACO) and the patient-centered medical home. These standards are derived from medical billing claims among commercial insurance companies along with the Medicare and Medicaid programs.
A presentation from Johns Hopkins Medicine explains that HEDIS quality measures should be used for quality improvement and serve to shape preventive care programs. Currently, more than 90 percent of health plans use HEDIS to determine their overall performance when it comes to serving their consumer base. Payers need to pay attention to a total of 80 measures within the HEDIS quality performance standards.
Payers need superior documentation
Documentation is vitally important when it comes to meeting HEDIS quality measures and improving payer performance. For example, now that the entire healthcare system has switched over to using ICD-10 codes, any claims that are sent in the form of ICD-9 or any other improper code will not count toward the quality standard.
It is also important to ensure a consumer or patient has all healthcare services properly documented in his or her electronic medical record. Any mistakes or errors within a medical record could be a major obstacle for meeting HEDIS quality measures.
Additionally, payers and providers will need to ensure certain deadlines for services are met in order to reach the standards of HEDIS. This includes preventive care such as ensuring immunizations are completed before a child’s second birthday.
Proper documentation within the medical record is key, as it follows the care of a patient and ultimately adds to high quality medical care. The electronic medical record allows physicians to further plan a patient’s treatment and monitor their vitals based on medications and procedures completed.
When it comes to filing medical billing claims and ensuring payment, the medical record is vital in providing a clear picture of all procedures and services completed. Such data could also be important for clinical research and further education within the medical industry.
Focus on patient care and preventive screenings
One payer HealthPlus of Michigan offered various several tips for providers looking to improve their HEDIS scores. First, it is important to determine which patients may need a well-care assessment by looking at gaps in care lists. Also, increasing access to healthcare services by addressing any scheduling or appointment issues is important when it comes to HEDIS quality performance.
There are plenty of preventive care measures that providers should meet including calculating adult body mass index levels, conducting mammograms and pap tests, completing immunizations, and managing hypertension and cholesterol.
Payers should partner with the type of providers who have high quality care and are meeting HEDIS quality measures in order to ensure their own health coverage plans offer superior service.
Incorporate population health management and patient engagement
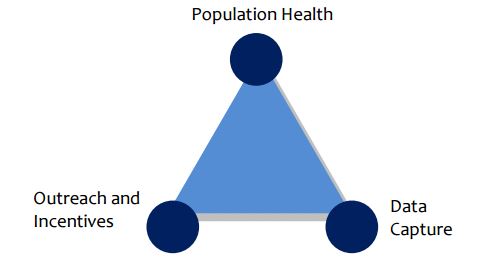
According to a report called Our Journey to Improve Quality and the Health of Our Population from the San Francisco Health Plan, payers would benefit from offering support to their provider network in the form of population health management strategies. Additionally, direct outreach and consumer engagement is encouraged by the health payer.
“SFHP credits part of our HEDIS success to our direct outreach to our members. Among the most long‐standing and effective interventions are the member incentive programs, where SFHP members receive gift cards for completing recommended care services such as annual well child visits or recommended tests for diabetes,” the report stated.
“Other interventions include live and automated phone call reminders for overdue care, and our ongoing work to provide health education materials and support for providers to teach patients how to manage their health and receive recommended care.”
With greater clinical data analysis and direct outreach to members recommending needed care, payers’ work with improving population health could directly improve their HEDIS scores, the report explains. HEDIS quality standards also focus on the patient experience, which means payers and providers will need to engage their patients by improving access to care and communication between patients and their primary care teams.
RevCycleIntelligence.com reported on the importance of patient engagement such as using patient portals to avoid having to schedule appointments but remain in constant contact with a primary care provider through secure messaging tools. This leaves doctors able to focus on more pertinent cases while patients don't waste time at unnecessary appointments. Patient portals are also useful in chronic disease management and prescription refills.
“We are really focusing on the Triple Aim as part of our business plan. If we’re struggling around the financial return on investment, let’s look and see if the other two elements of the Triple Aim – the patient experience and health outcomes – have been impacted by this program,” Dr. Margie Rowland, Chief Medical Officer, told RevCycleIntelligence.com.