Key Steps for Payers to Improve Population Health Management
Care coordination, disease management, and patient outreach remain the biggest obstacles for payers attempting to strengthen their population health management efforts.

- In recent years, population health management has become a larger factor in the success of a health insurance company. With more payers transitioning to value-based care reimbursement platforms, the quality of care and patient outcomes have grown in importance for both health plans and medical providers. As such, more payers have focused on improving population health management and targeting data analytics.

The New York City-based insurer Healthfirst is one example of a company that has used health IT and a health information exchange to strengthen population health management efforts. Rebecca Schwietz, Senior Vice President of Clinical Services at Healthfirst, explained some of the struggles that payers face in their population health strategies.
Care coordination, disease management, and patient outreach tend to be the key obstacles that payers address in their population health management improvements. When addressing care coordination and management, payers may find that their provider networks have far too many coordinators and patient navigators who lack needed communication channels and may overlap in their healthcare delivery. To solve this problem, payers should work with their provider organizations to ensure specific staff members are assigned to patients at risk of chronic conditions.
“Two important questions to ask (and answer) are: ‘Which members need care management support?’ and ‘Who is best positioned to provide that care management?’ Because members and their needs can change quickly, coordinating these two answers so that you can execute on them in a timely basis can be really challenging,” Schwietz said.
“We haven’t yet found the silver bullet here, but we are constantly working to improve our coordination with the many aspects of the healthcare system that supports our members,” she added.
Another example of a payer that’s brought more focus toward population health management comes from Humana, which has invested in more than 900 value-based, accountable care partnerships around the nation.
These structures span from patient-centered medical homes and pay-for-performance to full-accountability and shared savings arrangements, according to the Humana website. More than 1.6 million Medicare beneficiaries and 230,000 commercial members are served through accountable care partnerships at Humana.
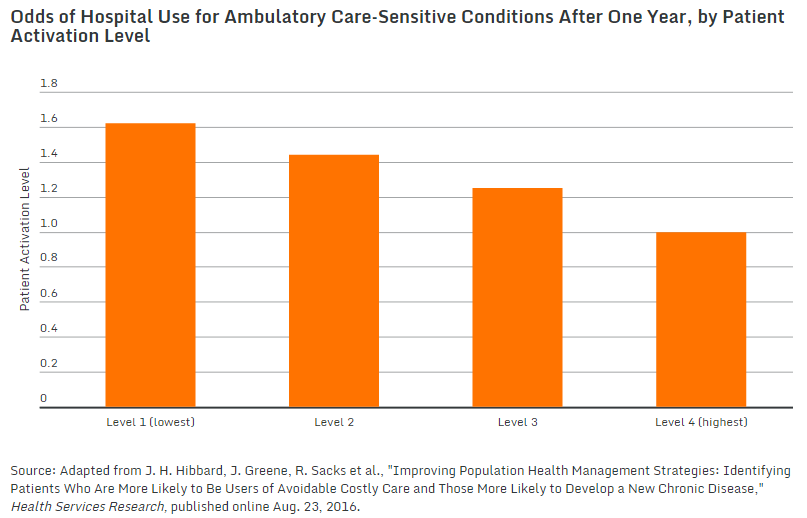
An additional solution that could assist with patient outreach difficulties payers face in their population health management strategy involves patient activation scores and population stratification. A study from the Commonwealth Fund outlines the importance of identifying patients more likely to be diagnosed with a chronic disease and participate in “avoidable costly care.”
The researchers looked at 98,000 patients and found that those who did not believe they could manage their own medical care had a higher likelihood of developing a chronic condition within three years than patients with better self-management skills. The researchers found that patients who had low levels of “activation” had a greater chance of hospitalization and emergency department use.
“The success of population health management depends, in part, on accurately identifying patients at high risk for poor health outcomes as well as preventable and costly health events,” the study authors stated.
“Risk-stratification approaches typically focus on clinical markers. This Commonwealth Fund–supported study explored whether considering a patient’s self-management skills and confidence—as predicted by the commercially available Patient Activation Measure (PAM)—might help health care delivery systems pinpoint additional high-risk patients who could benefit from supportive interventions. The Patient Activation Measure assigns patients a score of 0 to 100. Patient can be further grouped into four activation levels, with level 1 representing patients with the most limited self-management skills.”
Poor patient self-management was also found to be linked to higher rates of depression and blood pressure levels. Patients with the lowest activation levels had a 25 percent higher likelihood of developing a chronic disease over the following year than patients at the highest activation level. One year after beginning the study, patients with the lowest activation score had a 62 percent higher chance of being hospitalized compared to those with the highest activation scores.
The study suggests for stakeholders such as payers to stratify populations by patient activation scores in order to identify and assist patients with low levels of self-management skills.
Providers and payers can then pinpoint their patient outreach and attempt to improve activation levels so that these patients can become more capable in managing their own health. The researchers suggest for providers to recommend small steps of improvement for this sect of the patient population since too many changes may be unsustainable at the beginning.
When payers follow these steps in improving their population health management strategies, patient outcomes should progress and unnecessary medical costs should be reduced.
Dig Deeper:
Key Steps for Payer Success in Accountable Care Organizations
How Payers Should Prepare for Value-Based Reimbursement