How Payers Should Prepare for Value-Based Reimbursement
Payers and providers taking on value-based reimbursement arrangements must work towards reducing rates of hospital readmissions, hospital-acquired infections, and length of stay.

Source: Thinkstock
- Value-based reimbursement is a new payment strategy between insurers and providers meant to foster higher quality care by incentivizing strong performance with shared savings, bonuses, or other financial rewards. This diverges from the more traditional fee-for-service payment system in which providers are reimbursed based on the quantity of services instead of the quality.
Pay-for-performance is meant to stimulate a reduction in healthcare spending as well as bring improved health outcomes to the patient community. Payers and providers taking on value-based reimbursement arrangements often work towards reducing their rates of hospital readmissions, hospital-acquired infections, and length of stays in order to avoid penalties and meet quality performance benchmarks.
By moving away from fee-for-service payments, this alternative payment strategy incentivizes providers to utilize fewer services and, thereby leads payers to spend less on reimbursement.
No longer will wasteful and repetitive diagnostic tests plague the system. Value-based care allows payers to retain profit and spend less overall.
Additionally, value-based care is focused on preventive services and improving wellness. As such, it could ensure patients are healthier and in need of fewer medical services by encouraging medication adherence, healthy diets, and exercise among other lifestyle changes. When the patient population is healthier, payers will also be spending less on reimbursing providers. These are some of the reasons why health payers are becoming more and more interested in adopting value-based care reimbursement.
Dig Deeper:
What federal programs are promoting value-based care?
The Centers for Medicare & Medicaid Services (CMS) is bringing more focus toward value-based care reimbursement, as the federal agency has positioned half of all Medicare claims to be in the form of alternative, value-based payment models by the end of 2018. Currently, CMS is operating at least 30 percent of all their Medicare claims through an alternative payment platform, according to a news release from the Department of Health and Human Services (HHS).
Additionally, CMS established the Medicare Shared Savings Program several years ago, which brings new reimbursement structures for all accountable care organizations (ACOs) operating through the program. Essentially, ACOs must meet quality performance benchmarks and reduce healthcare spending in order to share in cost savings with the federal agency.
CMS has also created bundled payment programs that bring more focus on reimbursing episode-based healthcare instead of individual payment for each medical service found in fee-for-service models.
Starting in 1983, CMS established the inpatient prospective payment system, which covered all the costs associated with the entirety of a patient’s hospital stay.
More recently, the federal agency has introduced the Medicare Bundled Payment for Care Improvement (BPCI) program, which covers the costs of clinical episodes of care among hospitals, physician groups, and post-acute care facilities. The bundled payment covers all services beginning with an acute-care hospital stay.
CMS began this program in 2013 and selected a number of healthcare organizations to participate in this bundled payment arrangement, which consists of four new payment models. Bundled payments like this one promote value because these payment structures encourage healthcare providers to follow clinical guidelines and a specific set of services.
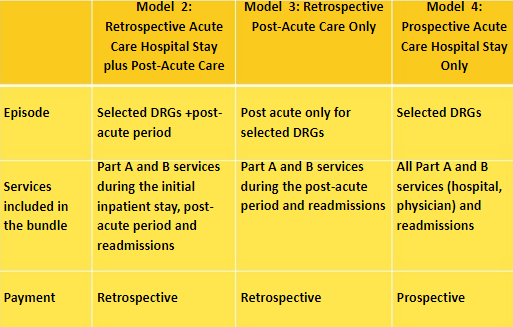
Source: Centers for Medicare & Medicaid Services
Starting on April 1, 2016, CMS began operating the Comprehensive Care for Joint Replacement (CJR) model, which manages the costs associated with hip and knee replacement surgeries as well as rehabilitation post-surgery. These federal programs are affecting private health payers who are beginning to position themselves in implementing value-based care reimbursement contracts. CMS has often been a leader in new healthcare payment strategies and this time is no different.
Dig Deeper:
- CMS Continues to Reform through Healthcare Bundled Payments
- What Are the Benefits of Accountable Care Organizations?
How can payers shift from fee-for-service to value-based care?
Payers will need to work with their provider network to develop new reimbursement contracts in which both payers and providers are satisfied with their new requirements and responsibilities. These new value-based contracts will need more focus on requiring providers to take on more financial risk as well as meeting quality performance improvements before receiving full reimbursement.
When it comes to value-based care, financial risk entails providers investing their resources in treating patients without a completely reliable outcome and essentially risking their own time and money in a process that could lead them to lose revenue if they don’t meet quality performance benchmarks with minimal services completed.
When health payers begin negotiating a contract and using a value-based care reimbursement strategy with their provider network, they may need to partner with providers more fully and ensure that clinical decision support tools are adopted throughout their provider network to help providers make cost-effective decisions about when certain services are warranted and when it might not be necessary.
For example, clinical decision support tools may enable doctors to receive the right guidance for ordering radiology studies, said Ryan Lee, MD, MBA, Director of MRI, Director of Quality and Section Chief of Neuroradiology, in the Department of Radiology at Einstein Healthcare Network.
“Clinical decision support is a great tool for clinicians ordering radiology studies."
"Previously, clinicians didn’t have any formal guidance,” Lee said. “They basically had anecdotal evidence that they may have had in their specific experiences and perhaps conversations with their radiology colleagues. There was no formal way for them to really get appropriate guidance for ordering studies.”
“We see that problem all the time because not infrequently patients would show up with the wrong studies being ordered, necessitating reordering of studies with new preauthorizations. With clinical decision support, this is will be changed,” explained Lee.
Further elaborating, Lee told HealthPayerIntelligence.com that clinical decision support tools play a role in eliminating waste, which aligns well with value-based care reimbursement protocols. Payers can work with their provider network to ensure these tools are being used to reduce wasteful spending.
“I think clinical decision support is that much more important in the value-based model because it eliminates waste. In the value-based model, waste is of high importance to eliminate."
"Clinical decision support allows a clinician to order the right test at the right time to minimize the wrong tests being ordered,” he pointed out.
Population health data also plays a vital part in supporting the health insurance industry’s transition to value-based care reimbursement. Payers attempting to better prepare themselves for value-based payment strategies should address population health management.
Health payers can use population health tools to define which patients are at higher risk of certain medical conditions or in need of preventive care. Essentially, payers can use population health data to better engage their consumers.
For instance, insurers can use data to target which consumers need a reminder to make an appointment for a wellness visit or a cancer screening. Payers can then send reminder notices in the mail and ensure their consumers are healthier and more engaged with their medical care.
Value-based care reimbursement aligns with providers taking on more financial risk, which relies on performance, health outcomes, and reduced hospital readmission rates. The Academy Research found by conducting a survey that, in 2014, 15 percent of healthcare services had transitioned to alternative payment models.
It is also important to remember that CMS has established goals to ensure that 50 percent of all their medical claims will be using a value-based alternative payment strategy.
Dig Deeper:
- CMS Innovation Center’s Role in Improving Value-based Care
- 5 Elements Essential for Value-based Care Reimbursement
How can health payers encourage downside risk sharing among providers?
Downside risk within the value-based care environment involves hospitals and medical facilities to risk any investment and resources when working with payers in a manner where their return on investment is below the expected amount. By utilizing downside risk, providers will be more incentivized to avoid redundant testing and medical errors, reduce their healthcare spending, and improve patient safety.
Health payers will need to work with their providers to ensure they are able to incorporate downside risk sharing in new value-based care contracts. First, it is important to outline with their provider network the various types of risk-sharing contracts available in the new value-based care reimbursement landscape.
The new strategies may include patient-centered medical homes, pay-for-performance models, shared savings, shared risk, capitation full risk, and bundled payments, according to a report from IDC Health Insights.
Payers will need to have access to quality and cost data in order to operate these new reimbursement models. Payers should express to the providers they’re partnering with the importance of quality improvement and the need to reduce healthcare spending through the adoption of downside risk sharing.
Many providers are looking for strategies that would reduce hospital-acquired infections, hospital readmission rates, and medical errors. Through downside risk sharing and value-based care, these goals can be accomplished.
Payers will need to continue collaborating with providers and improving their provider relations as well as bringing more contract management solutions to the table, said Jeff Rivkin, Research Director for Healthcare Payer IT Strategies at IDC Health Insights.
“To succeed in bundled payments [and value-based care], payers will need to prepare middle-office and back-office workflows and systems as well as involve multiple departments. Product management, plan management, and contract management are also advised,” Rivkin told HealthPayerIntelligence.com. “Other important factors to consider include care coordination/medical management, provider network management, and provider relations.”
Health payers are jumping on the bandwagon of value-based care reimbursement because it has a greater likelihood of cutting costs for the health insurance industry. Its focus on quality improvement as well as a reduction of wasteful, repetitive testing, hospital-acquired infections, and readmission rates all lead payers to save money and cut spending across the board.
The future of the healthcare industry as a whole is likely centered around risk-sharing and pay-for-performance. Whether it is found in federal programs or between payer-provider contracts, value-based care is here to stay.
Dig Deeper:
- How Risk-based Bundled Payment Arrangements Boost Quality
- The Role Risk Plays in Value-Based Care Reimbursement Models
