UnitedHealth’s Value-Based Care Reimbursement Improves Outcomes
UnitedHealthcare is one payer that has followed in the footsteps of CMS and adopted value-based care reimbursement models throughout their provider network.

- Value-based care reimbursement has been hitting both payers and providers as a surefire way to promote payment reform and reduce medical spending. The new models of payment are coming straight from public payers including the Centers for Medicare & Medicaid Services (CMS).

With a goal of having half of all Medicare payments to be in the form of alternative payment models by the end of 2018, CMS has been pioneering the healthcare industry’s move toward value-based care reimbursement. Currently, the public payer is operating about one-third of all Medicare payments in alternative, value-based models.
The more traditional approach to paying providers has often been in the fee-for-service reimbursement model, but this has often led to excessive use of medical care, unnecessary testing, and wasteful spending. As the healthcare industry moves toward reducing costs, value-based care reimbursement has been a major part of reforming the finances of this industry.
In recent years, CMS has been creating bundled payment programs such as the Medicare Bundled Payment for Care Improvement (BPCI) program, which consists of paying a number of providers based on an episode of care. This initially begins with an acute-care hospital stay and covers the costs of post-acute care facilities, hospitals, and follow-ups at physician offices.
CMS has also been incorporating value-based care reimbursement within the Comprehensive Care for Joint Replacement (CJR) model. This program covers the costs of hip and knee replacement surgeries among Medicare beneficiaries as well as the medical billing associated with rehabilitation after the operation.
All of these strategies adopted by CMS along with positive results have been stimulating private payers to also invest their time and resources in value-based care reimbursement. UnitedHealthcare is one such private payer that created a value-based program in which providers received bonus payments for improved performance.
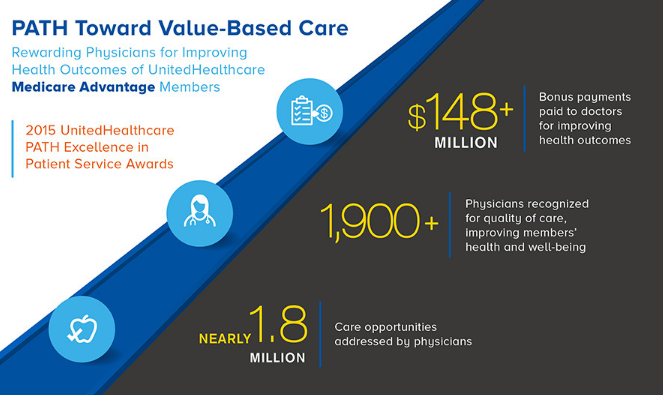
UnitedHealthcare announced in a press release earlier this month that it has awarded 1,900 providers with the 2015 UnitedHealthcare PATH Excellence in Patient Service Awards because these physician groups improved patient outcomes for those enrolled in the payer’s Medicare Advantage plans.
A total of $148 million in bonus payments was distributed among these providers for meeting the performance metrics required in the UnitedHealthcare PATH Program. UnitedHealthcare created this particular program in order to stimulate the utilization of preventive services among the provider community as well as increase monitoring of chronic medical conditions.
“The care providers who earned a PATH Excellence in Patient Service Award deserve recognition for their commitment to improving our plan participants’ health and well-being,” Efrem Castillo, M.D., Chief Medical Officer of UnitedHealthcare Medicare & Retirement, said in a public statement. “These awards are one of the ways we are supporting the transition to a value-based health care system that rewards physicians for the quality of care they deliver to the people we serve.”
The healthcare payer assesses which providers have met a number of performance-based measures including the Healthcare Effectiveness Data and Information Set (HEDIS) quality measures. Some of the ways in which providers improved outcomes and quality in order to receive these bonus payments include increased screening for breast and colorectal cancer among Medicare Advantage members as well as a rise in the number of diabetes patients who received an eye examination.
Additionally, these providers also gave out advice regarding how patients could maintain or improve their level of physical fitness. The providers were also responsible for closing gaps in care by ensuring that patients received all services and medications recommended for their age group. Just under 2 million care opportunities were garnered by those who participated in the PATH program.
The program first began in 2013 and has now expanded to serving almost 1 million Medicare Advantage members. Other healthcare payers looking to take part in value-based care reimbursement contracts may need to improve data exchange with their provider network as well as provide more support to physician practices looking to address care coordination.
In the move away from fee-for-service payments, payers will need to incentivize providers financially in order to have better performing networks. In order to embrace value-based care reimbursement fully, healthcare payers should work with their provider networks to determine what type of payment model works best for them.
Whether it is through accountable care organizations, bundled payments, or performance-based contracting, the move toward reforming healthcare payment is likely to benefit both the patient community and the health insurance industry.
Image Credits: UnitedHealthcare
Dig Deeper:
Key Strategies for Transitioning to Value-Based Care Payments
Why Payers Should Educate Providers on Value-Based Care