What Are the Benefits of Accountable Care Organizations?
Value-based care payment stimulates more preventive care and a reduction of hospital stays as well as emergency room visits.

Source: Thinkstock
- Accountable care organizations (ACOs) are provider and payer arrangements established to improve care coordination between primary care physicians, hospitals, specialists, and public or private health payers.
The Centers for Medicare & Medicaid Services (CMS), for instance, has created the Medicare Shared Savings Program in which accountable care organizations must meet quality performance benchmarks and reduce Medicare spending by a certain percentage point in order to qualify for sharing in these cost savings.
It is expected that ACOs will be capable of reaching quality improvement goals and reducing the costs associated with medical services by bringing greater focus to population health management.
However, accountable care organizations operating within the Medicare Shared Savings Program that do not immediately meet the quality performance benchmarks set up within the program may not qualify for sharing in the savings.
Dig Deeper:
Medicare Shared Savings Program Seeks High ACO Performance
What are the top challenges for accountable care organizations?
Lower reimbursement rates within the value-based care model including through the operation of accountable care organizations are bringing greater obstacles for healthcare providers. The traditional fee-for-service payment system brought in more reimbursement and incentivized physicians to order more tests and diagnostic procedures.
The way value-based care payment works is by incentivizing more preventive care and the reduction of hospital stays as well as emergency room visits. Additionally, there may be lower reimbursement rates as well as a lack of rise in physician revenue due to accountable care and value-based payments, according to the Practice Profitability Index report.
Even though there may be certain challenges when it comes to operating accountable care organizations, payers and providers are not letting that stand in their way as they continue to invest in new alternative payment arrangements and move away from traditional fee-for-service reimbursement.
HealthEdge’s State of the Payer Industry Survey showed that nearly 55 percent of polled medical establishments are looking to pursue ACO development over the next three years. The results also illustrate that four out of five surveyed organizations are looking to participate in value-based care reimbursement within the following three years.
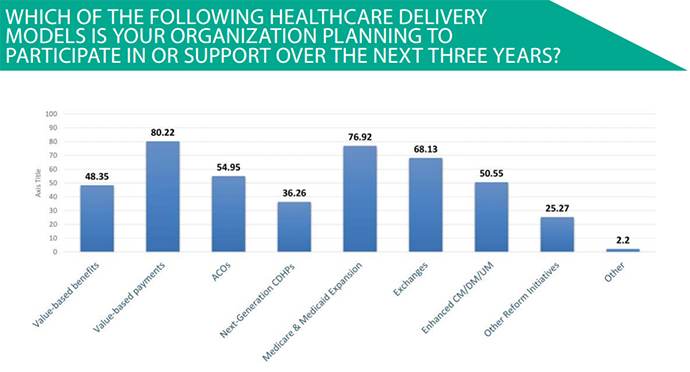
Source: HealthEdge
Dig Deeper:
- Top Challenges of Alternative Payment Models, Bundled Payments
- Value-based Payment Models Pose Challenge to Physicians
How can ACOs meet quality benchmarks and share in cost savings?
The first step that accountable care organizations can take in order to reach quality performance benchmarks is to put their time and resources in sticking with their investment. It is unlikely that ACO providers will immediately see results and cost savings when implementing this care coordination platform.
CMS has released results in the past showing that accountable care organizations which stay longer in the Medicare Shared Savings Program tend to have better results over time. Rome wasn’t built in a day and healthcare reform doesn’t happen overnight.
As such, it is imperative for ACOs to invest time and commitment in pursuing this model of care in order to see cost savings from the program. Amy Oldenburg, Vice President of Network and Product Strategy Accountable Care Solutions at Aetna, explained in an interview that “true transformation is a long-term endeavor.”
“We know that it takes at least three years for motivated ACOs to make changes necessary to impact real savings and quality improvements. We believe transforming health care will help reduce waste, improve quality, improve member/patient satisfaction, and improve overall employee health and productivity,” Oldenburg added.
“So we see this as well worth the commitment and investment of time and resources to get there. Through our approach to move providers and hospitals toward full, product-based risk-sharing ACOs and helping them transform the way they do business, we know we can help build a healthier world.”
Another important point to remember is that ACOs that adopt risk-based payment contracts are more likely to succeed in their endeavours because it brings more responsibility and financial incentive for physicians to truly change their best practices and improve quality performance in order to reduce healthcare spending.
Additionally, integrating risk-based contracts and value-based care reimbursement will benefit the patient community, as it is likely to enhance the quality of medical services. The Medicare Shared Savings Program, in particular, would function more effectively if more accountable care organizations embrace risk-based contracts.
Dig Deeper:
- Top 3 Ways Accountable Care Organizations Could Garner Savings
- Time, Commitment Required for ACO, Value-Based Care Success
How popular are accountable care organizations?
The results show that accountable care organizations keep proliferating throughout the United States. A study conducted by Leavitt Partners and the Accountable Care Learning Collaborative showed that the number of ACOs had grown 12.6 percent from January 2015 to January 2016.
At the beginning of this year, there were 838 ACOs found throughout the country while an additional 1,200 accountable care contracts are being created across healthcare organizations. The study also stated that more than 28 million patients are being treated by ACO providers today.
There is clearly a strong proliferation of accountable care organizations as the healthcare industry continues to reform and adopt value-based care reimbursement practices.

Source: Leavitt Partners and the Accountable Care Learning Collaborative
Health insurance companies are also seeking to partner with primary care providers and hospitals through an accountable care organization. For example, in early 2016, Aetna partnered with the Delaware Valley Accountable Care Organization and signed an accountable care contract.
The two parties hope to improve the patient experience and strengthen population health management all in an effort to reduce medical cost. About 70,000 Aetna members will be managed under the ACO umbrella due to this new partnership.
In February 2016, CMS also introduced 121 new ACOs to the Next Generation ACO Model and the Medicare Shared Savings Program. This shows that the number of accountable care organizations is on the rise across the nation as more medical providers and payers partner to reduce spending and improve the quality of care among the patient community.
Dig Deeper:
- Accountable Care Organizations’ Rise in Quality a ‘Home Run’
- Payers and CMS Seek to Join Accountable Care Organizations
What are the biggest benefits of accountable care?
The largest benefit that accountable care could bring for the healthcare industry is to garner cost savings or reduce spending. Healthcare reforms and new federal regulations whether it is the Affordable Care Act or the HITECH Act have all brought more focus on decreasing spending throughout the medical space.
The Affordable Care Act passed in 2010 positioned the development of accountable care organizations. Some healthcare experts find promise in ACOs and believe their biggest benefit will be in reducing the costs of care.
“I think that there has been some question to date because of the failure of Pioneer ACOs and the regular MSSP ACOs to show much cost savings but what folks have overlooked is that the ACO movement has been an organizing force throughout the healthcare industry and it’s got hospitals and doctors for once under the same umbrella talking about efficiencies, clinical protocols, and ways to save costs,” Ted Schwab, Managing Director at Huron Healthcare, told HealthPayerIntelligence.com.
“There are now north of 700 of these organizations in the United States of America. If you think about where the industry has been for the last 100 years, it’s been a mom-and-pop fragmented industry. Now you have 700 organizations with folks at least talking to each other. It’s going to take a while.”
“We’re at the very beginning of this movement and I could not be any more encouraged.”
For example, Blue Shield of California and its ACO provider were able to save $325 million over the last five years. The program was first begun in 2010 and has now expanded across 35 organizations treating as many as 325,000 patients in California. A key part of garnering these cost savings is through reducing emergency room visits and hospital admissions.
The number of hospital stays decreased by 13 percent and the number of days spent in the hospital dropped by 27 percent for the Blue Shield of California accountable care organization.
“We have achieved solid results in the first five years of our ACO program, and we are just getting started. We continue to deepen and refine the work we are doing with our ACO providers to ensure our members receive the right care at the right time and in the right setting, all the while helping to make healthcare more sustainably affordable,” Kristen Miranda, Blue Shield's Senior Vice President of Strategic Partnerships and Innovation, said in a public statement.
Another major benefit of ACOs is their ability to improve population health management and patient outcomes. A brief from the Center for Health Care Strategies and the Urban Health Research and Practice at Northeastern University shows that new healthcare delivery models like ACOs offer innovative methods for payers and providers to achieve better population health outcomes.
Medicaid ACOs, for instance, have shown a greater focus on preventing disease and promoting wellness, which leads to stronger population health improvements. This reduces the likelihood that a disease would progress and lead to more costly hospital stays.
The benefits of ACOs are numerous and there are many stakeholders who obtain advantages from this model of care. The patient community gains a wide number of advantages including improved outcomes, better quality of care, greater engagement with providers, and an overall reduction in out-of-pocket costs.
Health payers see significant cost savings from the program once risk-based contracts have been initiated. Healthcare providers are also bound to share in cost savings and benefit from a more successful population health management approach.
Dig Deeper:
- Blue Shield, Accountable Care Organization Saved $325 Million
- Population Health, Risk-sharing Vital for Accountable Care
